Nonspecific ulcerative colitis (UC) is a severe chronic pathology of the large intestine of an inflammatory-dystrophic nature, which has a continuous or recurrent course and leads to the development of local or systemic complications.
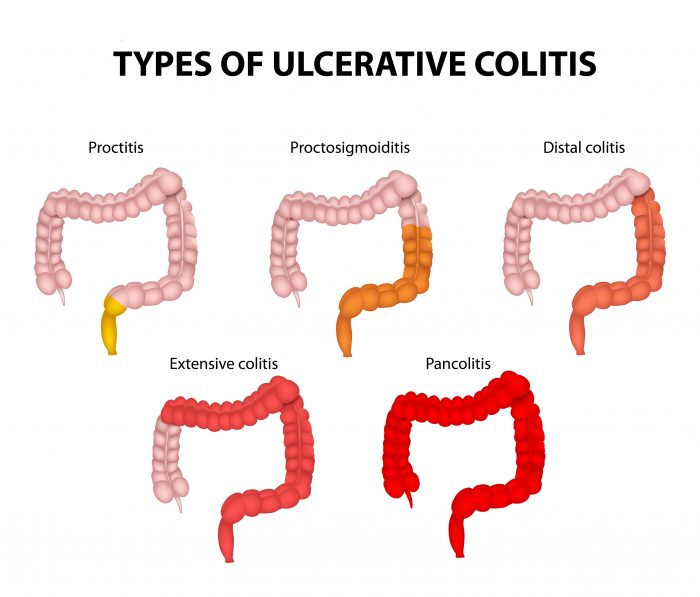
The process is localized in the rectum (ulcerative proctitis) and spreads throughout the large intestine. When the mucous membrane is affected throughout the large intestine, we speak of pancolitis.
The prevalence of the disease prevails among the population of industrialized countries. Over the past 20 years, there has been an increase in incidence not only in adults, but also in children of all ages.
UC can develop at any age in children, accounting for 8 to 15% of the total incidence. Infants rarely suffer from this pathology. At an early age, boys are more affected, and in adolescence, the disease affects girls more often.
Causes
According to the infectious theory, the trigger for the development of UC can be an infection, for example, salmonellosis suffered by a child.
Scientists have not been able to establish the exact cause of the development of UC. There are many theories about the etiology of the disease. Among them, the most recognized are:
- Infectious: according to it, the onset of UC can be provoked by:
- bacteria (for intestinal infections such as salmonellosis, dysentery, coli infection);
- microorganism toxins;
- viruses (for ARVI, scarlet fever, influenza).
- Psychogenic: the development of intestinal ulcers is provoked by stressful situations and psychological trauma.
- Immunogenic: the disease is caused by underdevelopment or failure of the immune system.
According to some experts, hereditary predisposition plays an important role - the presence of immune or allergic diseases in close relatives.
Damage to the mucous membrane by certain food ingredients and the iatrogenic effect of certain medications cannot be ruled out.
With UC, a whole chain of pathological processes occurs that are self-sustaining in the body: at first they are nonspecific, and then turn into autoimmune, damaging target organs.
Some scientists believe that the basis for the development of UC is energy deficiency in the epithelial cells of the intestinal mucosa, since patients have a changed composition of glycoproteins (special proteins).
Causes of the disease and its course
To date, scientists have not been able to fully identify the cause of this disease due to the difficulty of diagnosing intestinal microflora. But at the same time, some doctors believe that the frequent occurrence of stressful situations plays a significant role in the formation of ulcerative defects, while others, on the contrary, agree that a violation of the immune barrier contributes to the emergence of an imbalance of microflora and further damage to the integrity of the mucous membrane.
As a rule, when conducting genetic analysis and collecting a family history, it is often possible to identify the presence of immune or allergic diseases in a blood relative of the patient.
Avoid emotional stress
The reasons that can become an impetus for the development of the disease are:
- psychological trauma;
- constant emotional stress;
- excessive physical activity;
- the occurrence of an infectious disease, for example, scarlet fever or smallpox;
- SARS;
- development of acute intestinal infection.
Some scientists involved in the study of this disease believe that the main factor in the development of ulcerative colitis in children is a disruption of energy processes in the body, namely the formation of energy deficiency in the intestinal epithelial cells.
Unconditional proof of this theory is the identified changes in glycoproteins, which are present in absolutely all patients suffering from intestinal colitis. Often the inflammatory process develops in the descending parts of the large intestine and usually the rectum is involved in this process.
Ulcerative colitis in children has two forms:
- continuous;
- recurrent.
With the first, complete recovery is not observed, and periods of imaginary improvement in the condition quickly turn into an exacerbation of the inflammatory process.
The second stage is characterized by the presence of clinical remission after a period of exacerbation of the disease; the break between inflammation can last for several years.
There are also three clinical forms of ulcerative colitis:
- lightning;
- acute;
- chronic.
The first two are characterized by a rapid process and, fortunately, are observed less frequently in children, weeks in adults. Lightning-fast development of the disease can lead to the death of a child in 2-3 weeks.
Classification
Colitis is classified according to the location of intestinal damage:
- distal (damage to the colon in the final sections);
- left-sided (the process is localized in the descending colon and rectum);
- total (the large intestine is affected throughout);
- extraintestinal manifestations of the disease and complications.
There are different forms of UC in children:
- continuous, in which complete recovery does not occur, only a period of improvement is achieved, followed by exacerbation;
- recurrent, in which it is possible to achieve complete remission, which lasts for several years in some children.
There are such variants of the course of ulcerative colitis:
- fulminant (fulminant);
- spicy;
- chronic (wavy).
An acute and lightning-fast course is characteristic of a severe form of UC. Moreover, lightning can lead to death in 2-3 weeks; fortunately, it develops extremely rarely in children.
According to the severity, UC can be mild, moderate and severe. The activity of the process can be minimal, moderately expressed and pronounced. The disease may be in an acute or remission phase.
Kinds
According to morphological characteristics, colitis can be atrophic, catarrhal, ulcerative-erosive. If we take into account the nature of the course, the disease can be mild, moderate, or severe. By type it is divided into monotonous, latent, progressive and recurrent. According to the broadest classification, colitis is:
- primary;
- medicinal;
- nonspecific;
- parasitic;
- neurotic;
- nutritional;
- allergic;
- toxic;
- post-infectious;
- radial;
- spastic.
Symptoms and treatment of ulcerative colitis in children are almost the same as in other forms. At a young age, acute, chronic, nonspecific forms of the disease are often detected. The symptoms of spastic colitis in a child are as painful as with other types.
There is another classification of the disease. Since the large intestine includes several sections, colitis can have different localizations. According to this criterion, the following stand out:
- typhlitis;
- transversit;
- sigmoiditis;
- pancolitis;
- proctosigmoiditis;
- angulitis;
- proctitis;
- Typhlocolitis.
With any type of colitis in children, the symptoms are painful. If they appear, do not hesitate to visit a doctor. Timely treatment will improve your well-being in a short time.
Symptoms

Manifestations of the disease depend on the form and course, the severity of colitis, and the age of the children. The most characteristic symptoms of UC are diarrhea, blood in the stool, and abdominal pain.
The onset of the disease can be gradual or acute, sudden. Almost every second child develops UC gradually. In most cases, the stool is loose and foul-smelling, with the presence of mucus, blood (sometimes also pus). The frequency of stool varies - from 4 to 20 or more times per day, depending on the severity.
With a mild degree of colitis, there are streaks of blood in the stool; with severe colitis, there is a significant admixture of blood; the stool may look like a liquid bloody mass. Bloody diarrhea is accompanied by pain in the lower abdomen (more on the left) or in the navel area. Characterized by tenesmus (painful act of defecation), increased bowel movements at night.
The pain can spread throughout the entire abdomen. They can be cramp-like in nature, precede bowel movements or accompany them. Some children experience pain when eating.
Sometimes UC begins with the appearance of loose, loose stools, and blood and mucus are found in the stool after 2-3 months. With severe ulcerative colitis, body temperature rises within 38 ° C, and symptoms of intoxication appear. Sometimes a child is mistakenly diagnosed with dysentery. Exacerbations of the disease are regarded as chronic dysentery, and UC is diagnosed late.
Children with UC experience decreased appetite, severe weakness, bloating, anemia, and weight loss. On examination, rumbling is noted, and a painful, spasmodic sigmoid colon is palpable. The liver is enlarged in almost all children, and sometimes there is an enlargement of the spleen. In rare cases, constipation occurs with this disease. As the illness continues, abdominal pain occurs less frequently. Persistent pain syndrome is observed in complicated UC.
Complications
Long-term UC can lead to local and systemic complications.
Local complications include:
- Lesions in the anus and rectum:
- haemorrhoids;
- sphincter failure (incontinence of gases and feces);
- fistulas;
- cracks;
- abscesses.
- Perforation of the intestine and subsequent development of peritonitis (inflammation of the serous membrane of the abdominal cavity).
- Intestinal bleeding.
- Stricture (narrowed lumen) of the colon due to scarring of ulcers.
- Acute toxic dilatation (expansion) of the large intestine.
- Colon cancer.
In children, local complications develop in rare cases. The most common cause of any form of ulcerative colitis is dysbiosis (imbalance of beneficial microflora in the intestine).
Extraintestinal, or systemic, complications are diverse:
- skin lesions (pyoderma, erysipelas, trophic ulcers, erythema nodosum);
- damage to the mucous membranes (aphthous stomatitis);
- hepatitis (inflammation of liver tissue) and sclerosing cholangitis (inflammation of the bile ducts);
- pancreatitis (inflammatory process in the pancreas);
- arthritis (joint inflammation, arthralgia (joint pain));
- pneumonia (pneumonia);
- eye damage (episcleritis, uveitis - inflammation of the membranes of the eye);
When examining a child, you can identify manifestations of hypovitaminosis and chronic intoxication:
- pale skin with a grayish tint;
- blue circles near the eyes;
- dull hair;
- jams;
- dry, cracked lips;
- brittle nails.
Increased heart rate and arrhythmias are also noted, a heart murmur may be heard, and shortness of breath often occurs. With active hepatitis, yellowness of the skin and mucous membranes appears. The child lags behind not only in physical but also in sexual development. In teenage girls in the active phase of the disease, the menstrual cycle may be disrupted (secondary amenorrhea occurs).
In the chronic process, erythropoiesis (production of red blood cells) is inhibited, which, in addition to bleeding, contributes to the development of anemia.
After 8-10 years from the onset of the disease, the risk of a malignant tumor in the rectum increases by 0.5-1% annually.
Other features of symptoms
In the acute phase of nonspecific ulcerative colitis, the child’s bowel movements are disrupted. During bowel movements, the feces may contain blood.
Prolonged diarrhea leads to metabolic disorders and resulting weight loss. The child's appetite decreases and he refuses to eat.
There are a number of extraintestinal symptoms associated with complications of UC:
- Dysfunction of the cardiac system;
- Vascular lesions (thrombosis, thrombophlebitis);
- Impaired kidney and liver function.
Prolonged inflammatory processes in the intestines in children, left unattended by adults, lead to malfunctions in the systems and organs of the whole body, and therefore, without qualified medical care, they can cause disability.
Diagnostics
The doctor has to differentiate UC from diseases such as Crohn's disease, intestinal polyposis, diverticulitis, celiac disease, intestinal tuberculosis, colon tumor, etc.
UC is diagnosed based on complaints from the child and parents, examination results, and data from additional examination methods (instrumental and laboratory).
Instrumental studies:
- The main method confirming the diagnosis of UC is endoscopic examination of the intestine (sigmoidoscopy, colonoscopy) with a targeted biopsy for histological examination of the collected material.
The mucous membrane is easily wounded and edematous upon examination. At the initial stage of the disease, there is redness of the mucous membrane and contact bleeding, which is called the “bloody dew” symptom, thickening of the folds, and incompetence of the sphincters.
Subsequently, an erosive and ulcerative process is detected on the mucous membrane of the colon, folding disappears, anatomical bends are smoothed out, redness and swelling intensify, the intestinal lumen turns into a tube. Pseudopolyps and microabscesses may be detected.
- X-ray examination of the large intestine, or irrigography, is carried out according to indications. It reveals a violation of haustration (circular protrusions of the colon wall) - deformation of the haustria, asymmetry or complete disappearance, as a result of which the intestinal lumen takes on the appearance of a hose with smoothed bends and thick walls.
Laboratory research:
- a general blood test reveals reduced hemoglobin and a decrease in the number of red blood cells, an increased number of leukocytes, and an accelerated ESR;
- biochemical analysis of blood serum reveals a decrease in total protein and a violation of the ratio of its fractions (decrease in albumin, increase in gamma globulins), positive C-reactive protein, decreased level of serum iron and changes in the electrolyte balance of the blood;
- stool analysis for coprogram reveals an increased number of red and white blood cells, undigested muscle fibers, mucus;
- stool analysis for dysbacteriosis shows a reduced amount of E. coli, a reduction or complete absence of bifidobacteria.
Treatment
Treatment of UC must be carried out over a long period of time, sometimes several years. Conservative and surgical methods are used.
Conservative treatment should be comprehensive. The goal of the therapy is to transform a severe form of the disease into a milder one and achieve long-term remission.
The following are important for the effectiveness of treatment:
- adherence to the recommended diet;
- avoiding hypothermia;
- load limitation;
- prevention of infectious diseases;
- psycho-emotional peace without stress;
- avoiding overwork.
Since children with UC develop protein deficiency (due to blood loss) and loss of body weight, the diet should provide the body with proteins to compensate for its deficiency. Moreover, 70% of them should be animal proteins. The diet is recommended in accordance with table No. 4 according to Pevzner.
Optimal composition of the daily diet:
- proteins – 120-125 g;
- fats – 55-60 g;
- carbohydrates – 200-250 g.
The food consumed should be mechanically gentle. The supply of proteins will be provided by fish and meat dishes (in the form of soufflés and casseroles), fermented milk products, and eggs. Many children suffering from ulcerative colitis develop food allergies (most often to cow's milk). In these cases, all dairy products are excluded from the diet, only melted butter is allowed.
It is recommended to cook food by steaming or boiling in water or in a weak broth (fish or meat). Slimy soups are used as the first course. You can add meatballs, boiled meat, potatoes, and rice to the soup.
The child should be fed 5-6 times a day with warm food. From the menu you need to exclude foods rich in fiber, which increase intestinal motility and gas formation. Spicy foods and seasonings are also prohibited.
Jelly, fruit and berry decoctions (from pear, bird cherry, quince, dogwood, blueberry), strong brewed tea (black, green) will be useful, as they contain tannins and astringents. Coffee and cocoa are excluded.
In case of stable remission, a small amount of vegetables (zucchini, carrots, cauliflower, broccoli) is introduced into the diet. Tomatoes, melons, watermelons, citrus fruits, grapes, and strawberries are excluded from consumption. If well tolerated, you can give your child baked pears and apples, blackberries, blueberries, pomegranates, and cranberries. Chokeberry juice is very useful.
As a side dish you can cook potatoes, porridge (wheat, rice), pasta. Eggs (2-3 per week) can be given in the form of an omelet (steamed) or soft-boiled. It is allowed to eat white bread (day-old baked goods) and biscuits. Fresh baked goods and sweets should be excluded.
Expanding your diet should only be done in consultation with your doctor. The criterion for a correct diet and the effectiveness of therapy is the child’s weight gain.
The basis of drug treatment for UC is 5-aminosalicylic acid derivatives - Salofalk, Sulfasalazine, Salazopyridazine. A more modern drug is Salofalk (Mesacol, Mesalazine), which can also be used topically in the form of enemas or suppositories. As a basic therapy, a long course of Salofalk in combination with Wobenzym can be used. The dosage of drugs and the duration of the course are determined by the attending physician.
In case of intolerance to these drugs and in severe cases of the disease with extraintestinal manifestations, glucocorticosteroid drugs (Metypred, Prednisolone, Medrol) can be prescribed. If a child has contraindications to the use of hormonal drugs, cytostatics (Azathioprine) can be used.
If purulent microflora is cultured from the intestines, then antibacterial drugs are prescribed. To normalize intestinal dysbiosis, bacterial medications are used (Bifiform, Hilak-Forte, Bifikol, etc.).
Smecta, iron supplements, and wound healing agents (topically, in microenemas) can be prescribed as symptomatic therapy. Herbal medicines and homeopathic remedies (Coenzyme compositum, Mucosa compositum) can be used in treatment.
Indications for surgical treatment are:
- complications that arise (intestinal perforation, severe bleeding, intestinal obstruction);
- fulminant UC that does not respond to therapy;
- ineffectiveness of conservative treatment.
A subtotal resection of the large intestine is performed and an ileorectal anastomosis is performed (connection of the small intestine to the rectum).
Colitis in children: intestinal treatment
Any child's illness worries parents. They want to relieve the baby from pain as quickly as possible. Colitis in children is a common disease. Comprehensive information about the causes of its occurrence, symptoms, possible negative consequences, methods of treatment and prevention of relapses will help to provide immediate assistance to young patients.
In recent years, chronic diseases of the digestive system in children have increased significantly. About 20% of them are colitis - structural changes in the mucous membrane of the large intestine. It is accompanied by inflammatory processes and a characteristic clinical picture: pain in the abdomen, flatulence, stool disturbances, etc. Colitis in infants (up to 1 year of age) is called enterocolitis. In newborns, the disease often affects both the small and large intestines.
Doctors are unable to find out what causes enterocolitis in a child in the first months of life. It is known that allergic colitis in infants is associated with the inadequacy of some food products for the age category and its low quality. Inappropriate food and non-compliance with feeding regimens often cause allergies, which provoke colitis in infants. Among the factors of colon dysfunction in older children are:
- Acute intestinal infections. Dysentery, salmonellosis, etc. often cause dysfunction of the digestive organs.
- Intestinal infestations by worms. Parasites disrupt metabolic processes in the body, the functioning of the gastrointestinal tract, and destroy the epithelial layer of the intestinal walls.
- Increased emotional excitability, stress, and vegetative-vascular dystonia can provoke irritable bowel syndrome.
- Congenital intestinal anomalies, other pathologies caused by heredity.
- Radiation sickness as a consequence of radiation.
- Dysbacteriosis after unwise use of antibacterial, laxatives, and hormonal drugs.
- Deterioration of the local environmental situation.
- Gross violations of the rules of nutrition for infants: unreasonably early introduction of complementary foods, feeding newborns with whole milk.
- Autoimmune diseases. In some cases of malfunction, the child’s immune system fights its own organ tissues, destroying them.
- Allergies to drugs or food. Often the baby’s body reacts very sharply to certain bacteria entering the intestines from the outside. Medications used to treat various diseases disrupt the intestinal microflora.
Prevention
Preventive measures are aimed at preventing relapses of the disease. It is necessary to try to prevent the child from contracting intestinal infections that can provoke an exacerbation of UC.
You should not take medications without a doctor's prescription. Experts believe that drugs from the NSAID group contribute to the development of relapse.
An indispensable condition is compliance with the diet. Children must be provided with a protective regime: they are exempt from physical education lessons, labor camps and other stress. The best option is to study at home. Vaccination is carried out only according to epidemiological indications (after consultation with an immunologist) with weakened vaccines.
After discharge from the hospital, the child is registered with a pediatric gastroenterologist. If the disease lasts more than 10 years, annual colonoscopy with biopsy is indicated for timely detection of malignant degeneration of the intestinal mucosa.