The calendar shows the 35th obstetric week, the 33rd from conception, the 31st from delayed menstruation. There are only 5 weeks left until the expected date of birth (EDD).
- How do mother and fetus feel at this stage?
- What to expect from an appointment with a gynecologist?
- What dietary and behavioral features need to be taken into account?
What should alert a pregnant woman, read the article.
- Physical sensations at 35 weeks
- Ultrasound
- Vitamins
- Sex
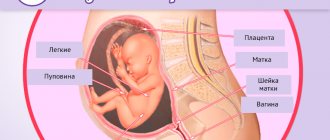
Fetus. Development at 35 weeks
Fetal development at the 35th week of pregnancy
At the 35th week of pregnancy, the fetus continues to grow and develop, rapidly gaining height and weight. Every day he becomes heavier by about 30 g and grows by several millimeters. Most often, babies at this stage weigh about 2.5 kg and stretch 46 cm in length.
It is worth noting that height and weight indicators are individual, and a significant deviation from these parameters is possible. During the entire third trimester, doctors monitor not so much the compliance of weight and height with the norms, but rather the rate of increase in these parameters in a particular baby.
After receiving the ultrasound results, the expectant mother should not look for norms on the Internet or medical literature; it is better to contact a specialist for clarification. Taking into account the parameters of the parents, the characteristics of the course of pregnancy and other factors, the obstetrician or uzologist will make a conclusion about whether the results obtained are normal for a particular fetus.
Active weight and height gain at the 35th week of pregnancy is the final stage of the gestational period. The main organs and systems have already reached the final stage of intrauterine development, the body has freed up resources to increase body weight and length.
Fetal growth this week increases due to the active development of tubular bones. Thanks to this, the limbs lengthen, the skeleton becomes proportional (like that of a newborn). Along with the increase in bone length, the process of calcium accumulation occurs. This makes them stronger, but they are still very flexible.
The flexibility of fetal bones is an important factor for a favorable delivery, provided by nature. The birth canal passing through a woman's pelvis is relatively small, its diameter is about 10 cm. The newborn's head (the most voluminous part of the body) is about 30 cm. During childbirth, the bones of the skull shrink slightly, allowing one to squeeze into the world outside the mother. This will not be possible if they are too hard.
If the mother was prescribed additional vitamin complexes containing calcium, they are often discontinued in the last weeks of pregnancy to avoid excessive ossification. But at the same time, the recommendation about a sufficient amount of this element in food continues to apply. If the doctor did not stop taking calcium-containing vitamins at your last visit, it is recommended to ask this question additionally.
The weight of the fetus increases this week due to the active growth of muscles and subcutaneous fat. Muscles are an essential component of the skeleton that ensures bone mobility. Their strength largely depends on the movements of the fetus. The muscles of the arms and legs are most developed at this stage. The baby will need to train most of the muscles after birth, gradually mastering conscious movements and subduing his body.
Subcutaneous fat of the fetus at the 35th week is represented by 2 types:
- white fat is a subcutaneous layer that acts as a thermostat and protects the baby from hypothermia. White fat does not yet work in the usual way for humans; it still has to develop and grow after birth, improving its function. The system for maintaining the most favorable body temperature (thermoregulation) will become fully operational only after 3 years; before that, control will be entirely on the shoulders of the parents;
- brown fat. This specific type of fat is typical only for babies. It is formed in the months before birth and is used in the first days of life. Its main purpose is to provide the newborn with the right amount of energy and nutrients during the acclimatization phase to the new world, while he sleeps a lot and eats little.
An increase in muscle volume and fat leads to changes in the appearance of the fetus: the skin smoothes and brightens, acquiring a natural shade. Lanugo (fluff) disappears over its entire surface, and the baby looks like a newborn.
The process of shedding of the vernix (lanugo) helps to wash away the vernix. She gave up her thermoregulation function to fat and by the 35th week she remained only in the folds of the body. Its remains will be used during birth to facilitate passage through the birth canal.
Another important process at week 35 is preparation for lactation. The maternal body triggers it thanks to the lactation hormone produced in the fetal adrenal glands. In addition, the fetus begins to take part in the production of the hormone-like substance prostaglandin, which is necessary to prepare the mother’s body for childbirth (softening the cervix, its shortening).
The baby’s entire endocrine system works well at this stage. The main glands are busy producing the necessary hormones and training their functions in a simplified manner. Immediately after birth, they will have to work hard, so they are already accumulating the necessary supply of substances.
The fetal immune system does not lag behind and continues to actively learn. The baby receives interferon from the mother's body through the umbilical cord, which promotes the formation of antibodies. The baby does not need this skill yet, he is in a sterile environment, but at the moment of birth everything will work at full capacity.
The gastrointestinal and urinary systems are best developed at this stage. They improve their skills daily using amniotic (amniotic) fluid swallowed by the fetus. It is successfully digested, dividing into necessary and unnecessary elements. A lot of discarded solid debris has already accumulated in the baby’s intestines (epithelial cells, pieces of lanugo, etc.), they will leave his body in the first days of life in the form of meconium. The baby's first bowel movements will be of an unusual color: black or dark green. The expectant mother should not worry, after 3-4 days the feces will turn yellowish.
The respiratory system is almost ready for active activity, but continues to accumulate surfactant (a substance to prevent the walls of the alveoli from sticking together during inhalation). All organs involved in breathing are in sleep mode, only the muscles responsible for raising the sternum during inhalation continue to contract and improve. This will continue until the baby is born, when oxygen from the mother’s body stops flowing, and the baby fills his lungs with air with his first cry.
If you evaluate the development of the toddler at the 35th week, you can note an incomparable transformation. In just 9 lunar months, a full-fledged person grew from a tiny cell (formed from mother’s egg and father’s sperm). There is very little time left before giving birth, but don’t relax. The expectant mother should still monitor her well-being and follow the doctor’s instructions.
Fetal movements and its position in the uterus
At the 35th week, the fetus occupies almost all the free space in the uterus, and it is difficult for it to turn over and move around. But despite this, he continues to pull himself up and stretch his muscles. Normally, within 12 hours a woman should feel about 10 movements, and count about 4 tremors in 1 hour in a calm position. It is recommended to monitor these indicators daily, so that in case of a sudden change in the baby’s behavior, seek help in a timely manner.
One of the aspects that worries the expectant mother and the gynecologist is the position of the fetus in the uterus this week. The most favorable position is considered to be cephalic presentation, when the baby is upside down.
If the position of the fetus is different at this stage, the woman is advised to stop wearing a bandage and consult with a gynecologist about the possibility of using techniques to turn the baby in the uterus. For now, the baby still has time to take the most favorable position for birth, but if he does not do this, then after the 38th week the question of the need for a cesarean section will be raised.
What happens to the developing fetus?
Fetus at 35 weeks of pregnancy
On the eve of the 35th week, even without complications of the ongoing pregnancy, expectant mothers should understand that the fetus has already practically formed and is in the position from which it will move during childbirth. The final stages of maturation of all systems and organs occur in the baby’s body. The weight of the fetus continues to increase weekly by almost 220 grams.
After the fetus moves towards the birth canal into the pelvis by the 35th week of pregnancy, the mother begins a period of decreasing pressure from the uterus on neighboring organs. She may feel less pain in the lower back and less frequent urination. It should be noted that this process may occur a little later, since each woman’s body during pregnancy has its own individual characteristics.
35th week of pregnancy what happens to the baby and mother
Mother. Changes in the psychological and physical state of the body at 35 weeks

The closer the expected date of birth (EDD), the more often the expectant mother thinks about this event. There are 3 to 7 weeks left before an urgent (full term) birth (from 38 to 42 obstetric weeks), but now many pregnant women are increasingly thinking about how this will happen, how painful it will be, and how they would like to organize the meeting.
A woman’s psychological readiness for childbirth is one of the components of successful childbirth. The expectant mother is recommended to master:
- breathing techniques to promote the birth of a baby and reduce pain;
- the ability to control your emotions, listen carefully to obstetricians. To do this, it is worth familiarizing yourself with the process of childbirth, understanding what will happen in each period;
- prepare for childbirth: collect all the necessary documents and things in advance.
Please note that in each maternity hospital the list of permitted things may differ, so as not to overpack your bags in the emergency room, you should find out everything in advance. It is most convenient to put the documents in a separate folder, which should be carried with you at all times during the current term.
List of required documents:
- maternity passport (+copy);
- compulsory medical insurance/voluntary medical insurance policy (+ copy);
- exchange card issued in hand at the antenatal clinic;
- insurance certificate of the state pension fund;
- birth certificate (if already received in consultation);
- referral to the maternity hospital (if any);
- agreement with the maternity hospital or doctor (if any).
When giving birth together with your husband, the list of necessary documents and certificates must be clarified at the maternity hospital.
It would be good to collect things in advance for your stay in the maternity hospital and for discharge. They should be placed in separate bags and signed. In one you need to put approved items for postpartum care, in the second - clothes for discharge. If you are planning a caesarean section, be sure to bring a bandage and elastic stockings.
Please note that the list of permitted items in different maternity hospitals may differ; it is advisable to ask in advance what you can and cannot take with you.
The discharge package must contain clothes for mother and baby. If you decide not to buy things before birth, then discuss with your loved ones what exactly they need to buy. Also think about your own outfit. Remember that immediately after giving birth, it is unlikely that you will be able to put on the clothes that you wore before pregnancy; your belly will disappear gradually, and in the first days it will resemble a deflated balloon.
By preparing things for the upcoming birth in advance, a woman will reduce her fear of the possible need to urgently go to the maternity hospital away from home. If necessary, she will simply go to the birth, and her loved ones will bring exactly what she needs.
The next change in hormonal levels that occurs in a woman’s body at the end of the period of bearing a baby can greatly affect the peace of mind of the expectant mother. In order not to be afraid of pain and the process of childbirth itself, it is recommended to attend special courses for young mothers, which discuss in detail the issues of childbirth and help cope with psychological difficulties.
Physical sensations at 35 weeks
In most cases, at the 35th week, the woman continues to experience familiar discomfort caused by the growth of the uterus and the enlargement of the fetus:
- frequent urination, sometimes slight urinary incontinence during sneezing or coughing;
- difficulty breathing: shortness of breath, feeling of constriction in the lungs;
- heartburn, flatulence, heaviness in the stomach, especially if the principles of a healthy diet are violated;
- back pain after walking or physical work;
- fatigue, drowsiness, some lethargy;
- itching of the skin of the abdomen;
- problems with sleep (difficulty finding a comfortable position, the baby is active, etc.).
Swollen breasts can also cause discomfort. Most women at this stage of pregnancy actively secrete colostrum from their nipples. Squeezing it or massaging the breasts is not recommended. This can trigger the production of oxytocin, a hormone that stimulates labor.
In some cases, as early as the 35th week, the process of lowering the abdomen may begin. This is how a woman’s body prepares for birth. If before this the stomach looked a little up, then gradually it begins to move the top to the bottom. This does not necessarily indicate an imminent birth, but if the belly is noticeably drooping, you should control your behavior, nutrition, well-being as much as possible, and get more rest. Nature provides at least 38 weeks for the baby to fully mature, so you should try to reach at least this period.
Along with the already familiar sensations, the expectant mother may notice the appearance of symptoms, which must be reported to the gynecologist as soon as possible. Before your appointment, it is advisable to take general blood and urine tests for a more accurate diagnosis. A pregnant woman should be alert to:
- burning or pain in the perineum during urination. Change in the color or clarity of urine;
- unpleasant sensations on the sides of the lower back, aggravated by tapping in the kidney area;
- the appearance of signs of varicose veins in the legs. Vessels are visible in the soft parts, star-like dots have appeared, etc. At the same time, the woman feels discomfort in her legs, especially in the evenings;
- discomfort in the back of the head, headache;
- exacerbation or appearance of hemorrhoids (pain in the anus);
- a sharp deterioration in appearance: hair loss, brittle teeth and nails, flaccid skin.
Visiting an obstetrician-gynecologist

At the 35th week of pregnancy, it is possible to schedule another scheduled appointment with a gynecologist. The day before, you need to take tests, directions for which were issued during your last visit to the doctor.
Women who have already completed the necessary studies for 3 screening usually undergo only general blood and urine tests, and, if necessary, a test for sugar levels and antibodies (if the pregnant woman has a negative Rh factor). Expectant mothers who, for some reason, have not previously been tested for biochemistry, HIV (AIDS), RW, hepatitis and hormone levels, need to do this before their appointment this week.
It is also worthwhile to undergo fetal cardiotocography (CTG) before appearing. Bring the results to your doctor for evaluation.
During the meeting, the gynecologist will conduct the usual measurements and surveys:
- will inquire about your well-being, ask about the emergence of new sensations;
- measure blood pressure, body temperature, heart rate of the mother (on the arm) and fetus (using a stethoscope);
- weigh the woman and calculate the weight gained since registration;
- will measure the abdominal circumference, the height of the uterine fundus, and compare the results obtained with the norm and past indicators of a particular pregnant woman.
At the end of the appointment, he will give recommendations (if necessary), set a date for the next meeting, and issue directions for blood and urine tests.
Ultrasound
At the 35th week of pregnancy, routine ultrasound is not provided as part of screening. It is carried out from 30 to 34 weeks. But, in some cases, if a pregnant woman has not been examined within the prescribed time frame, a referral may be issued. The study will establish:
- the condition of the fetus, its correspondence to the gestational age;
- position of the baby in the uterus (head, foot or transverse presentation);
- condition of the uterus, its cervix, placenta;
- presence/absence of visible external and internal pathologies of the fetus.
A woman who has undergone a screening ultrasound within the prescribed time frame can undergo an ultrasound examination on her own initiative for a fee.
Uterus and belly
At the 35th week of pregnancy, the fundus of the uterus is at a height of about 35-36 cm from the symphysis pubis, 15 cm above the navel. This week, the woman feels training contractions, during which the walls of the uterus contract, but do not cause pain. If the expectant mother feels pain during muscle contraction, she urgently needs to go to the maternity hospital.
The abdomen at this stage has a large volume and greatly affects the capabilities of the pregnant woman. It becomes uncomfortable to walk and move, and it is almost impossible to put on your shoes on your own. Many pregnant women experience severe itching over the entire surface of the abdomen, caused by skin tension. You should continue to actively care for your skin, using oils or a stretch mark cream recommended by your gynecologist.
This week, the expectant mother may notice that her belly begins to drop a little, her navel, which already protrudes well above her belly, begins to slowly move, looking not up, but forward. This event brings relief to the pregnant woman’s life: it becomes easier to breathe and eat. But the pressure on the bladder increases, and the number of visits to the toilet may become more frequent.
Pain in the abdomen and other parts of the body
Painful sensations at the 35th week in different parts of the body may appear within the normal range or indicate a possible pathology of pregnancy. The expectant mother should clearly understand what kind of pain should prompt her to seek medical help as soon as possible.
Signal for an emergency consultation with a gynecologist:
- pain in the kidney area when urinating;
- painful sensations in the legs not associated with walking or physical fatigue;
- headache, dizziness, heaviness in the back of the head;
- exacerbation or appearance of hemorrhoids.
Signal to call an ambulance or go to the maternity hospital:
- backache. The sensation is pronounced, the pain increases, does not go away at rest;
- abdominal pain. Drawing, cramping pain that increases regardless of body position;
- pain or pressing sensations in the perineum/thighs.
Discharge, bleeding, menstruation
Normally, vaginal discharge should have a slight odor, light or milky color, and an even consistency. At the 35th week, mucous lumps of an even structure may appear.
If the color of the discharge changes (yellow, green, gray), smell (pungent, unpleasant), consistency (flaky, curd-like), you should consult a gynecologist for advice.
If you experience red or brown vaginal discharge, you should immediately seek medical help. There should be no bleeding or menstruation normally during this period.
Excessively thin discharge is a cause for concern. If the expectant mother notes that the discharge has a watery structure, it is worth contacting a gynecologist as soon as possible or heading to the pregnancy pathology department.
Belly size at 35 weeks
The abdominal circumference at 35 weeks of pregnancy is approximately 88-92 cm.
The stomach has already become very large and causes a lot of inconvenience. At 35 weeks of pregnancy, the uterus became huge, pressing down on the stomach and lungs. At the end of the 35th week, the pregnant woman’s belly will begin to drop and breathing will become easier. If it becomes very difficult for the expectant mother to breathe, it is necessary to perform a special exercise for pregnant women, which will help reduce pressure on the internal organs: get on all fours and smoothly inhale and exhale. You can stand in this position from 5 minutes to half an hour, several times a day.
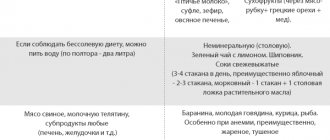
Nutrition

At the 35th week, some pregnant women will notice the beginning of the process of drooping of the abdomen, as a result of the body preparing for childbirth. For others, this change will begin a little later. As a result, women feel relief from digestion, but this is not a reason to break the nutritional rules. The uterus still puts pressure on the intestines, and a violation of the diet can cause constipation. It is worth adhering to moderation and some dietary features during pregnancy:
- split meals: eat 5-6 times a day, every 2.5-3 hours;
- finish your meal before you feel full;
- do not mix different dishes at one meal;
- limit food intake 2-3 hours before bedtime;
- drink about 1.5 liters of fluid per day, unless otherwise prescribed by the gynecologist;
- exclude all harmful products: smoked meats, pickles, semi-finished products, fast food, etc.;
- consume a minimum amount of salt;
- Do not drink strong tea or coffee unless otherwise prescribed by your gynecologist.
Vitamins
At the 35th week, most gynecologists suggest that pregnant women stop taking all multivitamins and dietary supplements, especially those containing calcium. It is recommended to strengthen control over the intake of essential nutrients from food, and to refuse those created chemically.
This is done so that in the last weeks, when the main development processes are completed, the fetus does not direct all unused resources into weight, thereby growing greatly. A large fetus is more difficult to deliver. If a gynecologist advises you to stop taking dietary supplements, it is better to listen to him.
Indications and contraindications for ultrasound
For an unscheduled ultrasound at 35 weeks of pregnancy, certain indicators are needed, namely:
- complaints of pain in the lower abdomen;
- bleeding from the genital tract;
- entwining the baby with the umbilical cord;
- suspicion of the presence of abnormalities in the child's development.
There are no contraindications to undergoing an ultrasound at 35 weeks. If the woman does not want to undergo the procedure for personal reasons, she may refuse the examination.
We recommend watching an overview video on the topic:
Weight
At the 35th week, the weight gained from the moment of registration of a pregnant woman can range from 8 to 14.5 kg. In some cases, deviations from these standards may be greater or lesser. Deciding how much the gained kilograms correspond to the term, whether there is a potentially dangerous underweight or overweight is the task of the gynecologist monitoring the development of pregnancy.
If a deviation from the calculated norm for a particular woman is detected, the doctor may recommend changes to the diet or suggest hospitalization.
It is possible and it is not possible

What is possible, what is not. By the 35th week of pregnancy, many rules of behavior are followed by a woman not so much out of necessity, but because there is no other option. Increased weight, increased fatigue, and difficulties in moving force the expectant mother to move smoothly, not make sudden movements, and think about her actions.
Pregnancy is approaching the end, but this is not a reason to relax. The goal of every expectant mother is to allow the baby to achieve maximum intrauterine development in order to be born fully prepared. To do this, you should continue to adhere to the basic principles of correct behavior:
- listen carefully and follow the gynecologist’s instructions;
- take tests and undergo prescribed studies in a timely manner;
- complete abstinence from alcohol, nicotine, and drugs;
- minimize contact with household and construction chemicals;
- proper nutrition and drinking regime;
- daily routine: sufficient sleep, daily walks, periodic warm-ups;
- careful body hygiene;
- order in the house;
- daily ventilation of the room in which the pregnant woman is located;
- minimal contact with possible carriers of viruses and bacteria;
- psychological calm.
Sex
Most gynecologists agree that at the 35th week it is worth limiting your intimate life. This is primarily due to the risk of premature birth. Unexpected movement, stress, or emotional upsurge can trigger the onset of labor, which cannot always be stopped within a medical facility.
Problems of the 35th week of pregnancy
At the 35th week of pregnancy, the main problems that a woman may encounter are:
- premature birth;
- pregnancy pathologies associated with both maternal health and abnormalities in the condition of the uterus and fetus.
Premature birth at 35 weeks is not uncommon. But in order for the baby to receive timely medical care, the expectant mother should know the symptoms of the process that has begun:
- constant pain in the abdomen, which does not stop at rest, gradually intensifying. Painful contractions - tension in the muscles of the uterus;
- aching and persistent pain in the lower back. In some cases, women may confuse the beginning of the labor process and ordinary pain after a walk. If the pain does not go away in a resting position, you should seek medical help;
- soreness or pressure in the hips or pubis. If it seems as if the pelvic bones are being pushed in different directions, you should call an ambulance;
- absence of fetal movements for more than 4 hours. A woman needs to sit down, calm down, count the kicks. If there is not a single shock within 30 minutes, go to the maternity hospital immediately;
- vomiting, intestinal cramps, diarrhea or frequent bowel movements. On the eve of childbirth, a woman’s body actively prepares, rejecting everything unnecessary;
- rupture of amniotic fluid.
There are a lot of options for pregnancy pathologies, and each of them should be observed by a gynecologist, and, if necessary, monitored in a hospital setting. For this purpose, there is a special department in the maternity hospital - pathological. If symptoms of a possible deviation from the norm are detected, it is recommended not to delay the decision and immediately go to the maternity hospital. The sooner the cause is identified, the better.
You need to go to the maternity hospital if:
- red or brown discharge appears;
- vaginal discharge is very liquid;
- gurgling sounds are heard in the area of the uterus;
- swelling of the arms, legs, face has appeared or intensified;
- there is a constant feeling of thirst;
- there is blurring in the eyes, fainting occurred.
If it is possible to get an appointment with a gynecologist on the day when a dangerous symptom was identified, you can first go for a consultation. But if the doctor recommends immediate hospitalization, do not hesitate.
35th week of pregnancy - there are 3 to 7 weeks left until delivery. More and more often, the expectant mother thinks about the future, feels better and better about her baby. The fetus gradually begins to reduce its activity, the mother’s belly begins to slowly descend, and mucous discharge appears from the vagina. The entire body of the expectant mother is being rebuilt, preparing for the upcoming meeting with her little son or daughter.
A woman should still adhere to the rules of behavior and nutrition for pregnant women, listen carefully to the gynecologist and follow his recommendations. A little more, and the long journey from the fusion of mother’s egg and father’s sperm will end with the birth of a new person.
If you liked the article, please share a link to it
What mothers write at 35 weeks of pregnancy
Last night, my right side suddenly began to hurt from the level of the navel and down to the pelvic bone. I couldn’t sit, I tried to get up - I can’t do it without help, I took a few steps - the pain was terrible in my side, I could only walk while bending over and holding my side with my hand. There is no way to bend over at all. I decided that this pain should go away lying down. She lay down on her back - there was a terrible pulling on her side, on the right side it felt like she was cutting with a dagger, on the left it was tolerable. It occurred to me that it was probably the intestines, constipation happens, and that during the day there was no stool, probably because of this. At night she only lay on her left side, did not get up, and you can say that she got enough sleep. But when I woke up in the morning, I began to get up with a slight pain on the right side; it was impossible to touch the area from the navel to the very side with my hand; there was a terrible pain when I pressed it. I got up, walked around, even cleaned the bed, and suddenly there was a sharp pain again. She lay down on her left side again. After a few minutes everything calmed down. I lay there for about 30 minutes, my son demanded breakfast, I had to get up... I lay down on my back and noticed that my stomach was just all twisted. Some kind of lumps all over my stomach... To reduce the pain I drank noshpa. It hurt a little less. She lay down again on her left side. The pain has calmed down. I re-read all the horrors on the Internet, and what scared me most was appendicitis... I still went to the toilet, freed my intestines, but the pain was no less... I think that right now my husband will come home from work, if it doesn’t get better, I’ll call an ambulance. But lying on my side I fell asleep, woke up, it was better, I could sit and even had dinner with my son. At 15.50 I went to do an ultrasound. See if everything is fine with the little one and check all your organs, find out what hurts!!! The ultrasound showed that our baby decided to turn around and lay down almost horizontally, that his head was on the left, and on the right where his back, spine, and butt hurt, his legs were down... the ultrasound specialist suggested that the little one was going to dive headfirst, but something was wrong and not it turns out. (We are in a breech presentation) We have ruled out the threat, the canal is closed, the cervix is 34 mm, there is plenty of water, there is no entanglement, what I could see of my organs is normal. The ultrasound specialist says that due to this position, the pain is caused by stretching of the uterus, ligaments and plus pressure on the intestines. In general, she reassured me that there was no need to run to the hospital. You need to be patient when he changes position. In two weeks, the baby gained as much as 1 kg of weight... And what will happen next... I imagine with horror that I will be in bed because of pain until the end of pregnancy... I immediately think, what if the ultrasound specialist didn’t see anything simple in me and this is really some kind of pathology with my intestines.. suddenly the appendix became inflamed and I don’t do anything about it... I was also surprised that I was able to sit down and drive for 2 hours to the dacha, but there I could barely walk, very slowly, so as not to hurt, and lay down again on my left side... So I lie on it... there is a slight pain when the baby moves... but it’s not sharp, it doesn’t sting, it’s aching... Touching the sore area is still unbearable... I think that it would be impossible to palpate the intestines through such a belly, or am I mistaken? After all, the pain sometimes radiates and can hurt in one place, but inflammation can be in another... What would you do in my place?