Children, like adults, often experience pain. A child may have a stomach, tooth, ear, or head pain. Pain is undoubtedly a reason to take your child to the doctor. But very often, pain begins to bother the child in the evening, at night and on weekends. What to do if a visit to the doctor is impossible at this moment? Can I give my child painkillers? In some cases it is possible and necessary, but in others it is strictly contraindicated. Which painkillers are allowed for children and which are not? It’s not easy for moms to figure this out on their own. I hope the article will help you with this.
What painkillers are suitable for children?
are used as painkillers in children .
- Paracetamol (single dose 10-15 mg/kg) and Nurofen (single dose 5-10 mg/kg) are used in children from birth (up to 3 months only on the recommendation of a doctor). Taken in the form of tablets, syrups, suppositories. They relieve pain for 2-3 hours.
- Nimesulide (single dose 1.5 mg/kg) is allowed for children from 2 years of age and relieves pain for 12 hours.
- It is allowed to use analgin as a pain reliever in children from 6 months, but only in the form of suppositories or intramuscular injections. Analgin tablets are allowed for children over 12 years of age.
Safe painkillers
Such drugs are produced in different dosage forms, each of which has its own advantages and disadvantages:
- Rectal suppositories. Compared to medications for oral use, suppositories are much less likely to cause nausea and other side effects, and do not put a strain on the digestive tract. The disadvantage of such dosage forms is that after administration it is necessary for the child to lie quietly for 10 minutes, otherwise the contents of the suppository will leak out.
- Pills. They have a clear mechanism of action and can relieve pain for a long time. The main disadvantage of such medications is their release form. For children under three years of age, painkillers should be crushed and given mixed with milk or water.
- Syrups. Sweet syrups with different flavors are the most preferred dosage form. They act quickly and are easy to use. The disadvantage of such drugs is the possibility of nausea or vomiting after administration.
- Ointments and gels. They are convenient to use, but have only a local anesthetic effect, so they are used only for injuries.
Painkillers for children
A child under three years of age is given analgesics in tablets, having first crushed the drug to a powder and diluted with water. For pain, they often use:
Article on the topic: Sildenafil - instructions for use, indications, composition, side effects, analogues and price
| Paracetamol | Ibuprofen | |
| Compound | paracetamol | ibuprofen |
| Action provided | has analgesic, antipyretic, weak anti-inflammatory effects | has analgesic and antipyretic effects |
| Indications for use | toothache, injury, migraine, high fever | neuralgia, symptomatic treatment of ARVI or influenza |
| Dosage (up to three years) | 0.5 tablets | selected individually |
| Method of administration | up to 4 times a day with water | up to 4 times a day with water |
Syrups
Sweet mixtures can be given to children under three years of age in pure form or diluted half and half with water. The following medications are preferred:
| Efferalgan | Nurofen | |
| Compound | paracetamol | ibuprofen |
| Action provided | reduces body temperature, eliminates pain | has an analgesic effect, reduces inflammation, reduces temperature |
| Indications for use | childhood infections, muscle pain, toothache or headache | |
| Dosage (up to three years) | weight up to 8 kg – 2.5 ml, from 8 to 16 kg – 5 ml | 30 mg/kg child’s weight per day |
| Method of administration | orally 1-2 hours after meals | |
External means
Ointments, gels, pain-relieving creams for children under three years of age are used for injuries. They quickly relieve pain, while the active substances are not absorbed into the systemic circulation. Preferred pain relieving ointments for children:
| Panthenol cream universal | Akriol Pro | |
| Compound | dexpanthenol | lidocaine, prilocaine |
| Action provided | soothes irritated skin, improves tissue regeneration, relieves pain | has a local anesthetic effect |
| Indications for use | injuries, burns | superficial anesthesia of the skin for injections, punctures and catheterization of blood vessels, superficial surgical interventions |
| Method of administration | Apply a thin layer to the affected area of skin | |
Suppositories
Can be used to relieve pain even in newborn babies. Suppositories are inserted into the child’s anus after bowel movements 1-2 times a day. Preferred pain relief suppositories for children:
| Viburkol | Viferon | |
| Compound | chamomile, plantain, belladonna, nightshade, meadow lumbago, calcium carbonate | interferon alpha-2 human recombinant |
| Action provided | has a calming, anti-inflammatory, anticonvulsant, antispasmodic effect | has antiviral, immunomodulatory properties |
| Indications for use | complex therapy of respiratory diseases, teething | acute respiratory viral infections |
| Dosage (up to three years) | 1 candle | 1 suppository |
| Method of administration | 2 times a day rectally | 2-3 times a day |
Not for children
- Aspirin is strictly contraindicated in children under 12 years of age.
- Citramon relieves headaches well if they are associated with low blood pressure. But citramon contains aspirin, so children under 12 years old should not take it.
- Andipal helps well when headaches are associated with high blood pressure. But, since it contains analgin, which is not recommended for children to take orally, Andipal is allowed for children from 12 years of age.
It should be remembered that pain cannot be relieved for a long time or permanently. It is allowed to remove it for 2-3 hours, maximum at night. But, as soon as possible, you should immediately visit a doctor.
Painkillers in pediatric practice
Author: Maria Andreevna in the section Medicines for children
Painkillers in pediatric practice
In order to treat children for pain, let's define the very concept of pain and whether analgesics should always be used. Pain is a border guard of health, a symptom that determines the dysfunction of one or another organ, and sometimes the whole organism.
Pain can be acute or chronic . The mechanism of acute pain is associated with irritation of nerve endings by biologically active substances released during cell destruction. Chronic pain accompanies serious illnesses and its manifestation is complicated by a violation of the neurotransmitter mechanism of pain perception in the brain.
Is pain a helper or an annoying discomfort?
Using well-known non-narcotic painkillers, we can only affect acute pain. But is this really necessary and in what cases is it permissible? In children, a rare process is accompanied by unbearable pain, which could not be relieved by maternal participation. But it always seems like it’s not enough, especially today, every mother has advertising pain relievers “Nurofen” and “Panadol”. But, besides the fact that a priori there are no safe medications, you should know that sometimes pain saves lives.
By removing pain with analgesics, we deprive ourselves of an indicator of the progress of the pathological process, receiving imaginary well-being. Without understanding the causes of pain and trying to relieve it, time is often lost, which can cost the child’s life. This situation may occur with abdominal pain. Banal childhood intestinal colic can result in intussusception, appendicitis, and Meckel's diverticulitis.
And when, it would seem, the child has calmed down and stopped thrashing about from “intestinal colic” while taking analgesics, the time for an irreparable tragedy comes. Pain in the stomach is not only not reasonable to treat with analgesics, but taking them aggravates the course of the disease and leads to erosive and ulcerative lesions of the mucous membrane . Therefore, the first rule:
- If you have abdominal pain, under no circumstances, without immediate examination by a doctor, do not give your child painkillers!
All that is permissible in this case is to give an antispasmodic agent (No-spa) and Simethicone preparations (Espumizan). If the pain is caused by spasm, overstretching of the intestinal wall by gases, then these two drugs will be enough to relieve pain. To relieve stomach pain, until you consult a doctor, it is permissible to take enveloping, antacid agents (Maalox, Almagel, Phosphalugel).
Analgin as the ancestor of non-narcotic analgesics
Today, in pediatric practice, it is permissible to use a very limited number of medications with an analgesic effect. These medications are not true analgesics; their analgesic effect is mediated by an anti-inflammatory effect. The exception is Analgin, but it is prohibited for use in pediatrics.
Metamizole (the active chemical substance of Analgin) is the only medicine from the group of non-steroidal anti-inflammatory drugs, which, in addition to the anti-inflammatory effect inherent in this group, has a direct analgesic effect. The analgesic effect of Metamizole is achieved by blocking the transmission of pain nerve impulses to the central nervous system.
In many countries, like Amidopyrin, Analgin has been discontinued. This is due to the high incidence of agranulocytosis during its use. Agranulocytosis is a pathological condition associated with the disappearance of neutrophilic leukocytes (granulocytes) from the blood. Granulocytes are the main fighters against pyogenic infection, therefore, with agranulocytosis, sepsis develops very quickly against the background of activation of its own conditionally pathogenic microflora inhabiting the oral cavity and intestines.
Read also: Solcoseryl gel for gums instructions for use
The cause of agranulocytosis is the damaging effect of Analgin (in particularly sensitive individuals) on the granulocytic blood germ in the bone marrow, as a result of which the flow of neutrophils of all degrees of maturity into the blood stops.
Analgin is part of a large number of complex medications under different trade names, for example, Sedalgin, Maxigan and others.
Aspirin is effective in both treatment and crippling
Other painkillers belonging to the group of non-steroidal anti-inflammatory drugs cause an analgesic effect by blocking the cascade of inflammatory reactions, which is triggered by biologically active substances released when cells are destroyed by some pathogenic agent. Aspirin (acetylsalicylic acid) should perhaps be considered the well-known ancestor of this group.
Aspirin has earned great popularity as a first-line antipyretic. A more effective and simpler antipyretic agent cannot be found. By reducing fever and inflammation, aspirin is also good at fighting pain. Who hasn’t heard: “Does your head hurt? Take aspirin, it helps.”
But, despite its advantages (availability and effectiveness), the drug is increasingly less often prescribed by doctors, finding its niche in the group of antiplatelet drugs. This is due to the high incidence of severe erosive and ulcerative lesions of the gastrointestinal mucosa.
And in pediatric practice, it was categorically prohibited to use it precisely for its direct indications: high temperature against the background of acute respiratory infections. The reason for this was the identification of Reye's syndrome. The essence of this syndrome was severe liver damage with aspirin taken to relieve fever caused by acute respiratory infections.
This combination of circumstances leads to acute liver failure, encephalopathy and death. Of course, not everyone develops Reye's syndrome, but it is impossible to identify children predisposed to it. Therefore, aspirin should not be used by children under 15 years of age.
Painkillers approved for use in pediatrics
Everyone knows about other drugs with an analgesic effect. Everyone knows Paracetamol and Ibuprofen.
Paracetamol is an active substance produced under different trade names by different manufacturers:
For pediatric practice, the drug is available in two dosage forms:
- - Syrup. 5 ml of the drug contains 120 mg of Paracetamol. Prescribed at the rate of 10 mg of the drug per 1 kg of child weight. To simplify calculations, each instruction for the drug contains a printout of the amount of suspension corresponding to the age of the child. Syrups must be accompanied by either a dosage syringe or a measuring spoon. The drug is prescribed from three months of age. It is prescribed up to 4 times a day with an interval between doses of at least 4 hours. It is not recommended to consume on an empty stomach.
— Rectal suppositories with paracetamol are produced under the trade names: “Cefekon” and “Efferalgan”. According to the recommended age group (from 1 to 3 months, from 3 months to 3 years and from 3 to 12 years) they contain different amounts of active substance from 50 mg to 300 mg. Suppositories are inserted into the rectum 2-3 times a day, preferably after stool, with an interval between administrations of at least 4 hours.
It is used primarily as an antipyretic, but can be used as an analgesic for moderate pain.
Ibuprofen. Better known by the trade name "Nurofen" or "Ibufen".
Available for pediatric practice in two dosage forms:
- - Syrups. Each 5 ml of suspension contains 100 mg of the drug. Ibuprofen is prescribed in the amount of 10 mg of the drug per 1 kg of the child’s weight. Each drug is accompanied by a dosage syringe with a printed table of the required amount of suspension, taking into account the weight and age of a particular baby. The medication is used 3 to 4 times a day at intervals of at least 6 hours, preferably after meals.
— Rectal suppositories are produced under the trade name “Nurofen” and contain 60 mg of Ibuprofen in each suppository. Prescribed for ages from 3 months to 2 years, one suppository 2-3 times a day with an interval of at least 6 hours.
Ibuprofen, compared to Paracetamol, has a more pronounced analgesic effect.
How do they work?
The mechanism of action of both Paracetamol and Ibuprofen is the same as that of the entire group of non-selective non-steroidal anti-inflammatory drugs. They block the enzyme cyclooxygenase (which is responsible for both the body’s inflammatory response and the blood supply and production of protective mucus in the gastrointestinal tract) and, due to this:
- - Stops inflammation. - Relieves pain. - Reduces fever. — Often cause erosive and ulcerative lesions of the gastrointestinal tract with bleeding.
Despite the fact that both drugs belong to the same group of drugs, paracetamol has some nuances of action and associated benefits of use, although very conditional.
It is believed that paracetamol interacts less with the enzyme cyclooxygenase within the mucous membrane of the gastrointestinal tract and therefore its ability to cause gastrointestinal bleeding is practically zero. But... we should not forget that it belongs to the group of non-steroidal anti-inflammatory drugs with a specific mechanism of action and chemical irritation of the gastric mucosa, which has not been canceled.
The most common undesirable results of their use
In addition to gastrointestinal bleeding and medicinal gastritis, the second, most common side effect of taking the drugs described is all kinds of allergic reactions of the skin and mucous membranes, from urticaria to severe epidermolysis.
Read also: How to use chlorhexidine for the oral cavity
Let’s also not forget about the possibility of developing agranulocytosis (and for some, pancytopenia), “aspirin-induced” bronchial asthma and kidney damage with the development of renal failure.
Complications are serious for such supposedly “safe” drugs and they do not occur in everyone and, of course, not all at once. But when deciding to relieve a child’s pain, it is always worth weighing the benefits against the risks experienced from self-administration of medications.
Alternative solutions for pain of different localizations
Sore throat, headache, and muscle aches often accompany infectious diseases with fever. And non-steroidal anti-inflammatory drugs used in these cases, reducing fever, simultaneously relieve pain. But you should not use this group if you have isolated symptoms. A healthy child should not have a headache, and if this happens, then it is necessary to find out the reason why the headache hurts, and not give analgesics.
To relieve sore throat with pharyngitis and tonsillitis of a non-bacterial nature, it is better to use absorbable tablets or sprays, for example, Imudon, Tantum Verde, used in children from the age of three.
If pharyngitis or sore throat is caused by a bacterial factor, then it is enough to choose the right antibiotic and the sore throat will go away on its own, without third-party intervention.
For pain from teething, it is better to use dental gels such as Cholisal or Kalgel. And it’s even better, if possible, to do without them.
If there is muscle, joint, or bone pain, it is necessary to first determine the cause of the pain syndrome, and then resolve issues of pain relief together with the attending physician. In the case of infectious-allergic arthritis, accompanied by severe pain, complex homeopathic preparations from Heel (Osteohel) can be used as an alternative to traditional treatment.
Or, which is better than self-medication, you can seek help from a homeopath of the classical school. But you should know that by leaving the walls of an official children's medical institution with a firm decision to “treat differently,” everyone takes responsibility for the health of their child.
Conclusion
To summarize the article, let’s take away the main points from it:
- — Pain is a physiological protective reaction of the body to a damaging factor. — When treating a child, it is necessary to begin not with relieving pain, but with finding out the cause of its occurrence. — There are no safe, absolutely harmless medicines. — In pediatrics, only two active ingredients (Paracetamol and Ibuprofen) are used as analgesics under different trade names. — There are alternative ways to relieve pain.
And remember, pain is always emotionally charged, adding sharpness to it. Parental involvement and the creation of a warm, caring atmosphere will reduce the intensity of pain and, in many cases, help avoid the need for analgesics.
Teething pain
All parents know about this pain. It can bother the child for several days and even weeks. The baby becomes capricious, sleeps worse, and eats poorly.
Help relieve teething pain
- During the day - special teething toys with water, which are recommended to be kept in the refrigerator before use. Cold reduces swelling and pain in the gums.
- Special gels for gums with local anesthetics, which are sold in pharmacies, help. For example, Kalgel, Cholisal, etc. These gels are applied to the inflamed areas of the gums after meals.
- If it is completely unbearable, especially at night, so that the baby falls asleep, you can give him the same Paracetamol or Nurofen.
Directions for use and dosage
It is recommended to drink 1-2 hours after eating with water.
Syrup
The syrup is enjoyed by children of all ages. It is prescribed from the second month of a newborn’s life. A dispenser is included with the medicine bottle. Syrup, which has a sweet taste, should not be diluted with water, but should simply be washed down with water.
The required doses for children are as follows:
- the amount of syrup for infants under 6 months is determined by the pediatrician, based on the baby’s weight and condition;
- from 6-12 months (2.5-5 ml);
- from 1-3 years (5-7.5 ml);
- from 3-6 years (7.5-10 ml);
- from 6-12 years (10-15 ml).
During the day, the medicine is taken four times, with an interval of 4 hours. In critical cases, admission is permitted more often, but only in a medical facility and under the supervision of specialists.
Candles
Suppositories are another form of Paracetamol. The suppositories are inserted into the child's anus. Due to their rectal administration, the active substance is absorbed into the intestines. The dosage of the suppository will depend on the age of the child:
- newborns up to 3 months as prescribed by a specialist if necessary, usually in a hospital;
- from 3-12 months 1 candle in a dose of 0.08 g;
- from 1-3 years 1 candle in a dose of 0.17 g;
- from 3-6 years 1 candle in a dose of 0.33 g;
- from 6-12, 1-2 suppositories at a dose of 0.33 g.
Suppositories are administered no more than 4 times a day, every 4 hours.
Pills
It is quite difficult for children, especially small children, to take it in pill form. Even if they are crushed into powder, not every child will be able to swallow this mixture. Tablets are allowed to be taken by children over 2 years of age.
The dosage of 200 mg tablets for children is:
- from 2-6 years – ½ dragee;
- from 6-12 years – 1 tablet;
- over 12 – 1-2 tablets.
Take no more than 4 times with an interval of 4 hours.
Paracetamol begins to work if taken with plenty of water. This applies to medicines in tablets.
When taken, the result is achieved within 30-60 minutes, and after three hours its effect ceases.
Pain in the mouth due to stomatitis
With stomatitis, ulcers appear on the oral mucosa, which cause severe pain, especially while eating.
Reduce pain from stomatitis
- To reduce pain, the same means are used as when teething: cold on the gums, pain-relieving gels.
- If the pain is unbearable, take nurofen or paracetamol orally.
- In addition, pureed, not hot, not spicy, not salty, not sweet food is recommended.
Local anesthesia in pediatric dentistry
Author: Stanley F. Malamed
The most important reason why children are afraid to have their teeth treated is the fear of injections (AlShareed, 2011). Parents/guardians should not focus on this before their child visits the dentist. When using topical anesthesia, good technique and distraction, most children are not even aware of the injection. Fear is a major indicator of poor pain management (Nakai et al., 2000). Before beginning any procedure, look for any red spots, rashes, or signs of injury to rule out an allergic reaction or avoid liability for damage that was already present before treatment. If something is discovered, it is necessary to invite and show the parent/guardian, and describe it in the medical history. Anxiety can trigger the appearance of a diffuse rash (Figure 2.1).

Figure 2.1 Diffuse rash caused by fear.
A reaction to medications taken may also appear in the form of a rash (Figure 2.2).

Figure 2.2 Possible allergic rash when taking penicillin.
The local anesthetic can be called a "sleepy drink". The little patient is told that his tooth will now fall asleep and then wake up, just as a child wakes up in the morning. The dentist or his assistant should observe him after the injection, waiting for the anesthesia to take effect. The rubber dam, in turn, is represented as a blanket that will cover a sleeping tooth. And after it is removed, the child is told that the tooth, lip and/or tongue will soon wake up. The time frame for when full sensitivity will return is not informative in this case for a small patient. It would be better to say that this will happen by lunch or dinner.
Infiltration anesthesia on the lower jaw leads to numbness of the lips, which can be unpleasant for the child. If possible, it is best to start by treating the upper molars to avoid discomfort and to help understand the sensation of local anesthesia before performing a wire, “switching off” lip and/or tongue. Parents/carers are advised that the numbness sensation may be more unpleasant for the child than the injection itself or the treatment itself. Typically, this is seen immediately after the rubber dam is removed and the patient complains that he is in pain (Figure 2.3).

Figure 2.3 Child immediately after treatment, upset about feeling numb.
A sticker reminding the child not to bite or suck in his lip and/or cheek should be placed on his clothing on the side of the anesthesia. Hot drinks should be avoided. These guidelines are provided to parents/guardians. You can also show them a photograph after biting the lip during anesthesia, and the child, if he is old enough to understand (Figure 2.4).

Figure 2.4 Swelling and bruising due to lip biting.
If damage to the mucous membrane occurs, vitamin E applications will help speed up healing. In the patient's chart, it is necessary to record the dose of anesthetic in milligrams, the place and type of anesthesia - infiltration, intraosseous or conduction, and the length of the needle (very short or short). The patient's response to anesthesia and recommendations given to parents/guardians should also be recorded (American Academy of Pediatric Dentistry, 2014).
Choice of local anesthesia
Bupivocaine, prilocaine, articaine, lidocaine and mepivacaine are amide anesthetics approved for use in pediatric dentistry. Bupivacaine is not recommended for young children or patients with mental or physical disabilities due to its long duration of action and possible risk of cheek or lip biting. Prilocaine should be used with caution, and its use should be avoided in children with oxygen transport disorders such as sickle cell disease, respiratory and cardiovascular diseases, or hemoglobin disorders, since one of the end products of prilocaine is methemoglobin, which reduces the capacity of hemoglobin carry oxygen (American Academy of Pediatric Dentistry, 2014). The peak level of methemoglobin in the blood occurs one hour after the injection, so children should be observed for at least an hour after using it. Gutenberg et al (2013) found no increase in methemoglobin levels with 2% lidocaine (1:100,000 dilution of epinephrine), which is very commonly used in pediatric dentistry. But the most common is 4% articaine. Prolonged numbness with a 4% solution may be of concern to children under 7 years of age. 40% noted discomfort after 3 hours and 11% after 5 hours. Biting of soft tissues, especially the lips, is common (Adewumi et al., 2008). The use of epinephrine at a dilution of 1:200,000 instead of 1:100,000 with 4% articaine should not change the effectiveness and is preferable for young patients. Meechan's study did not show a correlation between the effectiveness of buccal infiltration in the region of the mandibular first molars and the concentration of epinephrine in the solution (Meechan, 2011). It has been noted that 4% articaine is more effective in producing good anesthesia in infected areas and therefore may be the drug of choice for abscess removal (Kurtzman, 2014). The low pH of epinephrine, whether in articaine or lidocaine, can cause a burning sensation. Mepivacaine 3%, pH 4.5–6.8, does not contain a vasoconstrictor and may reduce discomfort after injection (Friedman, 2000). But, and therefore, rapid systemic absorption occurs. The maximum dose of 3% mepivacaine, 4.4 mg/kg, must be carefully calculated (American Academy of Pediatric Dentistry, 2014). Mepivacaine 3% may offer a good alternative for occlusal or proximal restorations in one quadrant in the primary dentition, with short procedure times and soft tissue anesthesia.
Dosage
Local anesthetic overdose was identified in 41% of insurance claims that involved the use of anesthetics in children. 43% of these cases were identified when only anesthetics were used among the drugs used (Chicka et al., 2012). In children, the cortical plate is thin and the bone is more vascularized, so local anesthesia occurs quickly. The use of a vasoconstrictor (epinephrine) reduces the risk of rapid systemic absorption and overdose. An anesthetic containing a vasoconstrictor is recommended for use when restorations are planned in more than one quadrant (American Academy of Pediatric Dentistry, 2014).
The dosage is calculated based on the child's weight and should never exceed the maximum. The maximum daily dose of 4% articaine with epinephrine 1:100,000 is 7.0 mg/kg or 3.2 mg/lb (Webb et al, 2012; Widmer et al, 2008; American Academy of Pediatric Dentistry, 2014), for 2% lidocaine with epinephrine 1:100,000 – 4.4 mg/kg or 2.0 mg/lb (Webb et al, 2012; Widmer et al, 2008; American Academy of Pediatric Dentistry, 2014). 4% solutions contain 40 mg/ml of the drug, and 2% - 20 mg/ml. One carpule contains 4% articaine – 68 mg. Although the carpool label says 1.7 ml, the actual volume is 1.76 ml, so it is more prudent to consider 1.8 ml when calculating the maximum dose. Label changes were made at the request of the Food and Drug Administration (FDA) when articaine (Septocaine) was introduced to the market in 2000. The 1.76 ml volume is suitable for all local anesthetics and one carpule of 2% lidocaine contains 36 mg. Most procedures for the treatment of primary molars are performed under infiltration anesthesia using 1/3 to 2/3 carpules of 2% lidocaine with 1:100,000 epinephrine. Treatment of pulpitis in the lower jaw may require conduction anesthesia with buccal infiltration, which will require from 2/3 to the entire carpule.
Discomfort during injection
Insertion of a needle results in discomfort from intraoral injections (Meechan et al., 2005). Amide topical anesthetics (lidocaine, articaine) quickly penetrate the systemic circulation and can contribute to overdose. They should be carefully inserted into the mucous membrane, dried with a gauze swab, and in a limited area where the needle is inserted (Figure 2.5a).

Figure 2.5 (a) Application of topical anesthesia for buccal infiltration anesthesia.
Anesthetics from a number of esters (novocaine, benzocaine) with a concentration of up to 20% are less absorbed into the circulatory system with a lower risk of overdose, but are also recommended only for use in small quantities (Kohli et al., 2000). The applied anesthetic must remain in the desired area for at least 2 minutes and is more effective on the mucous membrane than on the attached gum. A gauze pad is placed over the application site to avoid spreading or ingesting the medication and should be visible at all times (Figure 2.5b).

Figure 2.5 (b) 2 x 2 gauze pad after application of topical anesthesia.
Dental injection needles come in long (32 mm), short (22 mm) and very short (10 mm) thicknesses ranging from 23 to 30 g. There is no evidence of a difference in pain when using 25, 27 or 30 g needles for anesthesia in the maxilla or 25, 27 g in the mandible (Flanagan et al, 2007).
The advantages of thicker needles are less chance of breakage and less pressure required for aspiration. Injecting anesthetic through a 30-gauge needle requires more pressure, which can cause hydrostatic damage and increase the discomfort of the procedure (Kurtzman, 2014). A short needle injection can be performed if the soft tissue thickness is less than 20 mm (American Academy of Pediatric Dentistry, 2014). Short 27-gauge needles are preferable to 30-gauge needles for conduction anesthesia in the lower jaw in children. The direction of bevel of a 27-gauge needle toward or away from the mandibular ramus does not influence the effect of anesthesia in the treatment of pulpitis (Steinkruger et al., 2006). There was no reduction in injection discomfort when the anesthetic was warmed from room temperature to body temperature (Ram et al, 2002). Low pH levels between 2.9 and 4.4 may contribute to pain during the procedure and delay the onset of anesthesia. There is evidence that buffering the anesthetic, bringing it to a more physiological pH by alkalizing directly in the carpule before the procedure, can reduce discomfort and speed up the onset of effect (Malamed et al., 2013).
Inferior alveolar nerve block
It is believed that the highest percentage of intravascular injections involves inferior alveolar nerve blocks, for which 27-gauge needles are recommended. A long needle increases the risk of puncture of the venous plexus or artery, with increased potential for deformation or breakage due to unexpected patient movement (Figure 2.6).
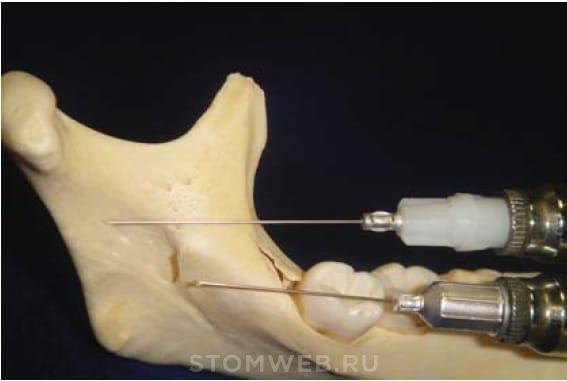
Figure 2.6 Comparison of long and short 27-gauge needles in the jaw of an 8-year-old child for conduction anesthesia to demonstrate the superiority of the latter.
Aspiration should be performed before and repeated during injection to avoid too rapid and intravascular injection (Malamed, 2011). The most important factor in preventing overdose is the speed of the procedure. The literature recommends a duration of 60 seconds for complete carpule insertion (Webb et al, 2012). The mandibular foramen is below the occlusal plane in the primary dentition and is level with it by 8.5 years of age (Figure 2.7).

Figure 2.7 Using a syringe to show the level of the mandibular foramen along the occlusal plane in an 8-year-old child.
As it grows, the vertical height of the jaw branch increases, so for insertion, the needle moves higher. In short-faced and elderly patients, the injection is placed further from the occlusal plane than in long-faced and younger patients. The anteroposterior location of the mandibular foramen is in the middle or two-thirds of the width of the ramus from its anterior edge (Epars et al., 2013). Injection of anesthetic below the orifice is a common cause of insufficient anesthesia (Malamed, 2011).
To block the inferior alveolar nerve, the doctor places his thumb on the coronoid notch, which is the deepest at the anterior edge of the ramus, and his index finger on the posterior edge of the ramus. Fingers can be swapped at the request of the doctor. The syringe is located at the opposite corner of the mouth parallel to the occlusal plane, at the desired level in accordance with the patient’s age. The anesthetic is injected two-thirds of the way between the thumb and index fingers (Figures 2.8a, 2.8b, 2.8c and 2.8d).

Figure 2.8 A (left) Technique for performing an inferior alveolar nerve block - the examiner's thumb is placed on the coronoid notch. B (right) The doctor's index finger on the posterior edge of the ramus of the jaw.
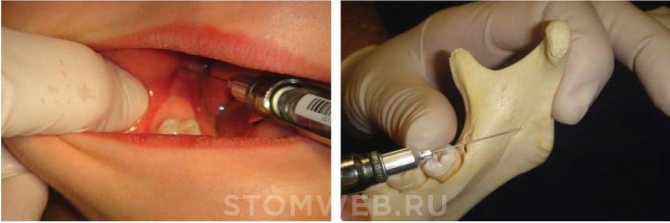
Figure 2.8 C (left) Inferior alveolar nerve block with syringe position relative to the occlusal plane in an 8-year-old child. D (Right) Shows the approximate position of the thumb, including soft tissue, with the inferior alveolar nerve opening two-thirds of the way between the thumb and index fingers.
Abstraction
It is necessary to talk to the child and keep the syringe out of his sight. Distraction with audiovisual glasses is effective in reducing pain during injection (El-Sharkawi et al, 2012) (Figure 2.9).

Figure 2.9 Audiovisual glasses to distract the child during local anesthesia.
During the procedure, you can ask the child to raise his leg, clench his teeth tightly during infiltration, or use a water-air spray from a puster and a saliva ejector, which also provide good distraction (Figures 2.10 – 2.12).
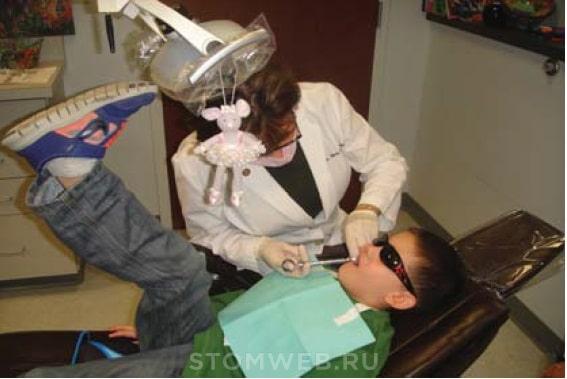
Figure 2.10 The patient raised his leg during local anesthesia.
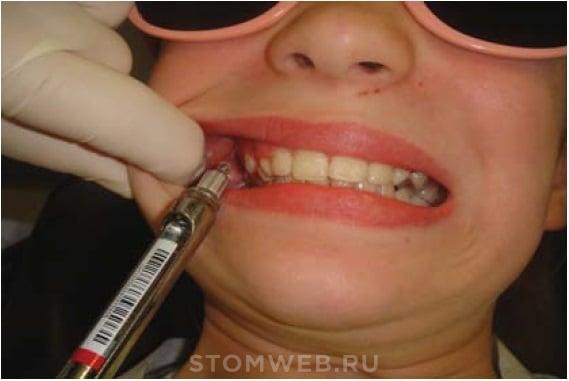
Figure 2.11 The child clenched his teeth during infiltration anesthesia buccally on the upper jaw.
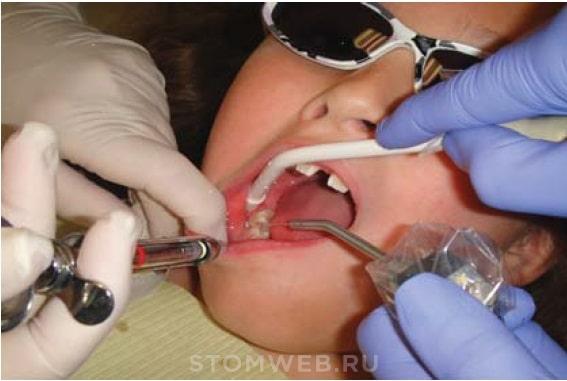
Figure 2.12 Water and saliva ejection from the side of buccal infiltration anesthesia on the lower jaw.
The DentalVibe™ (Bing Innovations) can significantly reduce needle anxiety and provide a more comfortable or painless injection by redistributing soft tissue tension with vibration. The device is wireless, rechargeable, backlit with an optical LED indicator and latex-free disposable tips that provide stretching with pulsating vibration and block pain (Figure 2.13).

Figure 2.13 DentalVibe™ device.
After informing parents/guardians about the need for treatment, the first question they often ask is: “Will I need an injection?” Demonstration and explanation of how DentalVibe works reduces their anxiety, which is often passed on to the child, and results in less stress for everyone. The device is not well accepted by children under 4 years of age, but is very effective in reducing anxiety in adolescents, in the author's experience. Ching et al (2014) also noted a significant reduction in pain when using DentalVibe during anesthesia in adolescents. Discomfort from injections is palatally reduced in patients of all ages. Mandatory demonstration of the device must precede the injection. Topical anesthesia is necessary to reduce discomfort from needle puncture of soft tissue. The needle is inserted next to one of the contact tips of the device (Figures 2.14 and 2.15).

Figure 2.14 DentalVibe™ for buccal infiltration.

Figure 2.15 DentalVibe™ for palatal infiltration.
Removal of mobile primary incisors or molars can be performed quickly and essentially painlessly using topical anesthesia supplemented by a DentalVibe, which is placed adjacent to the crown of the tooth (Figure 2.16).

Figure 2.16 DentalVibe™ in addition to topical anesthesia for the removal of a very mobile primary tooth.
Daria Elina
Headache
For infection
- Preschool children most often have headaches due to viral and bacterial infections. When body temperature rises.
- But sometimes the temperature is not very high, up to 38 C, and the child complains of a severe headache. To remove it, you can give the child the same paracetamol or nurofen or nimesulide.
- In addition, the mother needs to know that a headache during an infectious disease (for example, the flu) is one of the signs of intoxication. To relieve intoxication, a child needs to be given intensive water and regularly ventilated.
For schoolchildren
Headaches in schoolchildren and adolescents most often occur during the school year, when children are at school. During the holidays, the number of schoolchildren complaining of headaches decreases. This is due to stress at school and at home. Especially often, conscientious students - excellent students who sit until late at night studying and then don’t get enough sleep - get headaches.
Headaches in schoolchildren are often associated with changes in the tone of blood vessels and a decrease in blood pressure.
To completely get rid of such a headache you need
- Set up a daily routine for your child.
- Remove unnecessary loads if possible.
- Make sure that the student takes regular walks.
- To have sufficient physical activity.
- Limit the time spent on the computer and TV.
- Make sure that the student goes to bed no later than nine to ten o’clock in the evening.
If this is not enough, and the headaches continue, you urgently need to show the child to a pediatrician and neurologist.
But it is possible to relieve such acutely severe headaches in children for several hours. All the same: Paracetamol, Nurofen, Nimulid.
Headache after injury
If your child has a severe headache after an injury (for example, a blow to the head). Especially if it is accompanied by lethargy, lethargy, and vomiting! You cannot give painkillers to your child. You need to call an ambulance or urgently take the child to the doctor.
Painkillers for infants
Can I give my child painkillers? Adherents of naturalness are confident that the unpleasant symptoms of any infant disease can be stopped with the help of maternal affection alone, but their arguments are unlikely to seem convincing to those whose baby is crying because of teething or colic in the stomach. Is it worth solving the problem with analgesics, or would it be wiser to look for an alternative to medications?
Indications for the use of painkillers for children
Over the past few years, the pharmaceutical industry has made great strides, thanks to which many painkillers have appeared in pharmacies that can be safely given even to infants. Most of these drugs additionally contribute to:
However, even a special medicine for newborns can cause harm to a child’s fragile body if its help is used too often. You can’t do without such tools when:
Each of the listed cases is a direct indication for giving the baby painkillers. When should you not do this?
When is taking painkillers contraindicated?
That is why it is very dangerous to arbitrarily give any drugs to children complaining of headaches or abdominal discomfort. These symptoms may be signs of:
Does your child often have a headache or stomach ache, but the examination did not reveal any health problems? In this case, parents should consult with their doctor about choosing an appropriate analgesic. Only a specialist will be able to determine which drug will be safe for a particular child.
What requirements must pediatric painkillers meet?
Basic requirements for such drugs:
- quick effect;
- long-term exposure without accumulative effect;
- low risk of adverse reactions;
- Availability of a dosage form suitable for children.
Which analgesic release form should I choose for my child?
Which form of medication to choose depends on the age of the child:
| Age | Recommended dosage form | Advantages |
| Up to 3-6 months | Rectal suppositories (suppositories) | There is no risk of injuring the sensitive gastrointestinal tract |
| 1-7 years | Liquid (syrups, suspensions) | Easy to give to children thanks to a wide range of flavors and aromas, no difficulty in swallowing |
| 7-12 years | Tablets, powders | High concentration of active ingredient, easier to choose the right dosage |
The best pain medications for newborns and older children
Determining which children's pain reliever is best is difficult. According to international clinical studies, the most effective analgesic for babies is Ibuprofen, but it can only be used when the child reaches six months. Paracetamol, which is in second position in the rating, is allowed from 3 months, but an overdose is fatal.
To choose the analgesic that is most suitable for their child, responsible parents will have to comprehensively study the modern pharmaceutical market. What painkillers are there?
- Efferalgan, Panadol and other paracetamol-based suppositories. They have a pronounced antipyretic effect. They can be used from birth, but they should only be used as prescribed by a doctor.
- Viburcol. Fast-acting homeopathic suppositories based on herbal ingredients. Have no side effects. Good for pain caused by teething.
Non-drug methods for eliminating pain in children
In cases where the use of analgesics in one form or another is contraindicated for a child, parents can use alternative methods to relieve an attack of pain. For children under 3 years of age it will help:
- light relaxing massage;
- method of switching attention;
- ethnoscience.
With older children, you can try breathing exercises and various relaxation exercises. The main thing is to create maximum comfort for the child, make sure that he empties his bowels in advance, takes a comfortable position and completely relaxes.
Diseases, injuries or natural teething are accompanied by painful sensations. A baby experiencing an unpleasant symptom begins to cry loudly and the parents’ task is to alleviate his suffering. Analgesics for children will help cope with this task.
Products for children
To help the child, painkillers are used without waiting for a doctor’s recommendation. Fortunately, the analgesic is sold in every pharmacy.
When giving analgesics to children, it is important to adhere to the instructions, observing the dosage, maintaining the required interval between doses of the medication.
Analgesics relieve pain, reduce fever, relieve swelling and other manifestations of the inflammatory process.
It is necessary to give the child analgesics in the following cases:
- ARVI, otitis media, influenza, accompanied by fever, pain in the head and abdomen;
- eruption of baby teeth;
- disruption of the gastrointestinal tract;
- colic, increased gas formation (in infants);
- injuries;
- exacerbation of congenital pathology.
The drugs have antipyretic, anti-inflammatory, analgesic effects. The mechanism of action is due to inhibition (inhibition) of the synthesis of prostaglandins - mediators of pain, inflammation, hyperthermic reaction. The platelet concentration does not increase, which reduces the risk of blood clots. The effect of the analgesic lasts from 4 to 12 hours.
- convenient dosage form: gel, ointment, mixture, suspension, solution;
- minimum contraindications, side effects;
- the ability to quickly and permanently relieve pain;
- the active ingredients are removed without accumulating in soft tissues.
When a baby in his first year of life cries and screams, he needs the help of his parents. Having correctly calculated the dosage, the following forms of analgesics are used:
- for newborns who still have difficulty swallowing, rectal suppositories are placed: Efferalgan;
- starting from 6 months, they give aromatic sweet syrups, suspensions: Paracetamol, Nurofen, etc.
- Rectal suppositories rarely cause nausea or other side effects. After insertion, the child is fixed in a position lying on his side (for 10 minutes), squeezing his buttocks.
- suspensions, syrups - convenient forms of analgesics, taken after meals;
- tablets, powders act quickly and for a long time;
- ointments, gels have a local analgesic effect;
- sprays help with burns;
- lozenges;
- drops.
Tablets, powders, capsules are prescribed to teenage children. If Paracetamol tablets are prescribed to a child under 3 years old, the analgesic is crushed to a powder state. Before giving, stir with water.
When the baby is teething, his suffering is alleviated with the help of external analgesics. To do this, rub an ointment or gel (Kalgel, Cholisal, etc.) into the inflamed gum.
For itchy skin, infants and older children are prescribed a cream or spray: Bepanten, Panthenol.
Syrups are an analgesic for children from six months. Children take the aromatic, sweet drug with pleasure. Sometimes the analgesic in syrup form causes nausea.
Safe pain relievers include rectal suppositories. Because suppositories are inserted into the anus. In addition, the risk of side effects is minimal.
List of the most popular drugs
Paracetamol (Panadol, Efferalgan, etc.) – relieves headaches, toothaches, pain after injury, relieves fever and inflammation. Suitable for babies from 3 months. It acts in 20 minutes, achieving effect in half an hour. The effect lasts almost 6 hours.
Ibuprofen (Nurofen) – in the form of a suspension is approved for children from 3 months. No less effective than paracetamol. It has a pronounced analgesic and antipyretic effect. The use of NSAIDs is prescribed during teething. The analgesic takes effect 30 minutes after administration, and the effect is achieved after 2 hours.
Nimesulide (Nise) – suitable for children over 2 years of age. Calculated: 1.5 mg/kg. The active substance works in 30 minutes, the effect is achieved in 1.5 hours. The analgesic lasts for 12 hours. Prescribed for injuries and teething. Not suitable for reducing temperature.
When should you not give painkillers to children?
The use of analgesics is strictly prohibited if the following conditions are detected:
- liver diseases;
- hormonal imbalances;
- constipation causing abdominal pain;
- poisoning: nausea, diarrhea, vomiting and other symptoms;
- predisposition to allergic reactions;
- abdominal pain of unknown origin;
- head injury;
- severe sore throat;
- purulent discharge from the ear;
- gums are swollen, teeth hurt, cheek is swollen;
- at the same time: headache, drowsiness.
Adverse reactions after use
- abdominal pain, vomiting;
- loss of appetite, flatulence;
- decreased hearing or vision;
- headache, sleep disorder;
- hives.
Traditional methods of pain relief
- to relieve fever and muscle pain, rub with vodka;
- pain from a bruise will be relieved by a compress of grated horseradish and honey;
- the headache will go away if you apply a fresh, pre-crushed cabbage leaf.
Few people think that pain relief does not solve the problem, but sometimes leads to serious complications. The pain syndrome does not appear on its own, but signals that there has been a malfunction in the functioning of the small organism.
Therefore, before using such products, the child is shown to the pediatrician.
Source: https://rody-beremennost.ru/lechenie/obezbolivayushhie-lekarstva-dlya-grudnichkov
Contraindications or when not to use painkillers for children
- Any abdominal pain.
- Severe headache after injury. Especially accompanied by vomiting and episodes of loss of consciousness.
- Discharge from the ear is a contraindication to instilling ear drops into the ear.
You need to call an ambulance or immediately take the child to the doctor if the child has
- Severe unbearable headache and repeated vomiting.
- Headache and he is lethargic, sleepy and difficult to wake up.
- Headache and he loses consciousness.
- He has a very severe pain in his throat, he cannot open his mouth and has difficulty speaking.
- Acute pain in the abdomen.
- It started leaking from my ear.
- The tooth hurts and the cheek and/or gums are swollen.
All of these cases indicate that the child is most likely already experiencing serious complications of the disease. His condition requires urgent medical attention.
SIMILAR ARTICLES:
- Drug overdose in children Drug overdose in children...
- Pancreatitis in children Acute Chronic Pancreatitis in children is quite common...
- Baking soda for a child For rinsing Baking soda can be used for a child...
- Fukortsin for a child with chickenpox Fukortsin, like brilliant green, is local...
- Nasal drops for children What are possible? When a child has a runny nose, mothers look for...
Contraindications to the use of analgesics
Analgesics in childhood are prescribed according to strict indications, but there are conditions in which their use is also strictly contraindicated. These conditions include:
- headaches after head injury or unknown etiology,
- acute pain in the abdomen,
- ear discharge,
- individual intolerance to the drug,
- unreasonable use (for minor pain),
- exceeding the daily dose.
Elimination of pain in some surgical and neurological pathologies can hide the most striking symptoms and lead to diagnostic error.
In addition to these conditions, there are medications that are absolutely contraindicated for use in pediatric practice. These include:
These drugs can cause serious complications in children. Therefore, they are shown only after 12 years.
The child's body is too fragile and unstable. Therefore, the prescription of any drugs must be strictly justified and approved by a doctor. If any adverse or allergic reactions occur, you must discard this drug and replace it with another.