Vulvitis in girls is an inflammatory disease that refers to pathology of the external genitalia. These include the labia majora and minora, the vestibule of the vagina, the clitoris, and the opening of the urethra also opens.
This is one of the most common diseases in gynecological practice; almost every girl, regardless of age, faces this problem.
The risk group is the age of children from one year to 7 years, when the pathology occurs most often. In addition, it requires immediate treatment, since the consequences can be very serious and in some cases lead to changes in reproductive function.
Etiology
The main reason for the development of vulvitis as a given disease is tissue damage by microorganisms or fungi. Bacterial flora can be completely different, both specific and non-specific.
Factors contributing to the inflammatory process:
- Foci of chronic infection. These can be either severe systemic diseases or simply a long-term persistent infection. Such pathologies include damage to the urinary system, digestive tract, endocrine pathologies, especially those that disrupt metabolism in the body. The most common cause is infectious diseases of the upper respiratory tract and pharynx.
- Helminth infestation of the body, in particular the rectum . These could be roundworms or pinworms, which, affecting the area of the external opening of the direct passage, spread to the vulva area.
- Entry of foreign objects , this can be accidental or intentional. Most often it occurs in young children who play in the sand or in the sea, most often without panties. Particles of dust, dirt, sand, etc. get onto the surface of the vulva or inside the vagina, which provoke an inflammatory reaction.
- Decreased immune system , this can be caused by autoimmune diseases or viral etiology, as well as long-term use of antibacterial agents.
Particular attention should be paid to the appearance of such a common type of inflammation of the vulva of an allergic nature, which occurs against the background of increased sensitivity of the body to environmental factors:
- It can also be the consumption of specific foods such as chocolate, citrus fruits, etc. The use of personal hygiene products containing dyes, fragrances and irritating components.
- Too frequent and incorrect use of diapers, diapers, personal hygiene products . And also in combination with them with powders, ointments or napkins.
- Failure to comply with the rules of personal hygiene , this can be either too frequent or, conversely, infrequent washing with the wrong technique.
Causes of itching
Often girls in adolescence are faced with the problem of scabies in the intimate area. There can be many reasons for this. Among them are the following:
- weakened natural defenses of the body;
- possible presence of colpitis in the body;
- venereal diseases;
- nervous tension;
- thrush and other infections;
- uncomfortable underwear;
- unsuitable personal hygiene products.
Itching in the intimate area is a signal from the body that some kind of malfunction has occurred. The reasons can be very diverse. First of all, this is a change in the hormonal background of adolescents during the restructuring of the body. Treatment is carried out in stages, in a course, using hormonal drugs. Additionally, douching and herbal baths are done.
The second most common cause of itching in a child is poor personal hygiene. Often this is improper or infrequent washing of the genitals. Redness and irritation appear on the skin. To relieve inflammation, use conventional hygiene products (soap, gels) or antiseptics.
Allergic reactions can also cause itching in the intimate area in girls. This mainly affects children aged 2 to 3 years. The cause of itching can be soap and diapers. Before treatment, the allergen is first removed. Sometimes the use of antihistamines is required.
Itching of the intimate area can be caused by tight or synthetic underwear. Girls' bodies are growing daily. Therefore, it is necessary to ensure that your underwear is updated frequently. You need to be especially attentive to children under 4 years of age. Kids cannot always make it clear that their underwear has become tight and uncomfortable.
Another cause of itching in the intimate places of girls is inflammatory processes in the vaginal mucosa. Even children as young as 5 years old can be susceptible to this. Their private parts begin to itch very much and this is immediately noticeable. Colpitis often occurs in girls, but it is difficult to notice it at the first stage. After delayed treatment, complications may occur, such as infertility.
Itchy private parts are sometimes a consequence of the development of diabetes mellitus, a malfunction of the thyroid or gonads. Relief usually occurs after hygiene procedures. Treatment is carried out by an endocrinologist, and it is necessary to consult a doctor as quickly as possible, without delaying time.
The cause of itching is vulvitis. The disease manifests itself as inflammation of the external genitalia. Pathology can be observed even in five-year-old children. Less common - in children under 5 years of age. The main causes of vulvitis are chemical or mechanical injuries, inflammation or infections.
A rare cause of itching is pubic lice. They appear only in adolescents, since insects require hair to move. Therefore, before the age of 13, itching due to pubic lice usually does not occur. When insects appear in the hair area, severe itching begins. To prevent lice, bedding should be changed frequently and personal hygiene should be maintained. To remove insects, it is enough to shave the intimate area well several times.
Another important problem that causes many diseases, including itching, is stress. Teenagers are especially susceptible to them during puberty.
Stress can cause excessive emotional or physical stress, prolonged depression, and fatigue. All this provokes nervous itching. Treatment requires conventional sedatives; no additional drugs are prescribed.
Classification
Depending on the type of development, as well as the duration, vulvitis in girls should be divided into several groups:
- Acute inflammation (usually lasts up to 1 month)
- Subacute inflammation of the vulva (duration can be several months, periodic extinction or exacerbation of symptoms is observed)
- Chronic (symptoms of the disease may worsen over several years)
Depending on the factors that caused vulvitis in girls:
- Bacterial vulvitis
- Fungal vulvitis
- Non-infectious vulvitis (Trauma, chemical damage, allergic nature)
According to the mechanism of infection:
- Primary. In direct contact of the pathogen with the body.
- Secondary. Persistence of the pathogen in the body, chronic infections.
Types of vulvitis according to the age period during which inflammation occurs:
- Vulvitis of newborns.
- When the child is under one year of age.
- Vulvitis of childhood.
- Prepubertal vulvitis. Until the first period appears.
- Vulvitis of puberty.
Signs and symptoms
The symptoms of vulvitis in children are in many ways similar to other genital infections (colpitis, vulvovaginitis).
Signs of the disease:
- burning and itching;
- pain in the genital area, which becomes more intense when urinating;
- swelling and redness of the clitoris, labia, vulvar mucosa;
- Sometimes there are erosions and ulcers on the mucous membrane.
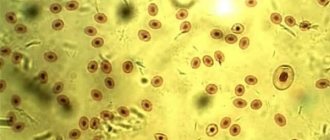
Vulvitis in girls is characterized by vaginal discharge (leucorrhoea). They can be different, depending on the type and cause of the disease. They are mostly clear, but can sometimes be purulent or bloody. If the cause of the disease is E. coli, the leucorrhoea has an unpleasant fecal odor and a greenish-yellow color. If the infection develops when the vulva is affected by staphylococci, they are viscous and yellow. Vulvitis of a fungal nature is accompanied by a cheesy, white discharge.
READ ALSO: Symptoms and first signs of rotavirus infection in children: treatment and prevention of dirty hands disease
Sometimes the disease may be accompanied by general symptoms:
- temperature increase;
- enlarged lymph nodes;
- nervousness;
- sleep disturbance;
- irritability.
If vulvitis is caused by pinworms, girls' anal folds thicken and redden, abdominal pain appears, and appetite worsens.
When the disease becomes chronic, swelling and hyperemia become less pronounced, but itching and leucorrhoea persist. With relapses of vulvitis, complications may develop in the form of cystitis, cervical erosion, urethritis, and vaginal atresia.
Symptoms of vulvitis in girls
Most often, the disease occurs acutely; little time passes from the moment of exposure to the pathogen, therefore the incubation period is not prolonged.
After penetration of the pathogen or its contact with the skin, symptoms of vulvitis begin to quickly appear:
- First of all, the main symptoms include redness of the external genitalia , the intensity usually directly depends on the severity of the pathological process. It can be either slightly hyperemic, but sometimes bright burgundy in color. Subsequently, it is accompanied by gradually increasing swelling. In the most severe cases, it can provoke a violation of the outflow of urine.
- Swelling causes severe itching. Up to scratching and the addition of additional infection, maceration and development of cracks.
- Also one of the specific symptoms is discharge from the genital tract. They can look different, their nature depends on the type of pathogen, they are light or have a greenish, yellowish tint, usually with a fairly liquid or creamy consistency. With candidiasis in nature, they have a thick consistency, reminiscent of cottage cheese; it can also be flaky and white.
- The smell is almost always unpleasant , sometimes sour.
- The child begins to behave restlessly, cries often, is constantly bothered by itching, and severe scratching occurs. Sleep and general behavior are disturbed, appetite decreases.
- In some cases, especially with a specific infection, body temperature may increase. Rarely, other systems may be involved, so urination may become more frequent, accompanied by severe pain and cramping. Some children complain of abdominal pain.
- Upon examination, you can also see enlarged lymph nodes , especially the inguinal group.

Diagnosis of vulvitis in girls
Diagnostic stages:
- First of all, the diagnosis of vulvitis is based on communication with a gynecologist , he clarifies the complaints, the time of their appearance, as well as factors that could contribute to the appearance of the pathological reaction.
- The allergy history and cases of specific infections among family members, as well as hygiene methods that are used, are clarified.
- A thorough examination of the child is carried out. Initially gynecological, followed by examination of the anus, as well as all body systems. The lymph nodes are palpated.
- In some cases, vulvitis requires a two-handed digital rectoabdominal examination. This is important if the doctor has doubts about the degree of development of the pathological process. An assessment of the internal genital organs, the degree of their development and involvement in the inflammatory process is carried out.
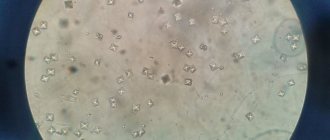
- Among the laboratory research methods for vulvitis, the study of smears is used , onto which the contents of the discharge are applied. Sensitivity to antibacterial agents is also determined for more accurate selection of treatment.
- This is also a general or, if necessary, urine test according to Nechiporenko.
- Examination of stool for worm eggs is one of the important studies. Especially when the picture of the pathological process is unclear.
- In severe physical conditions, a blood test is also performed to assess the degree of the inflammatory process.
- If necessary or if a specific infection is suspected, the vaginal contents are examined using the PCR method.
- If candidiasis is present, an examination is carried out for the presence of glucose in the blood and urine .
- In addition, one of the instrumental methods to assess the extent of damage is ultrasound examination of the pelvic organs.
Treatment
The regimen will depend primarily on the general condition, as well as the severity of the inflammatory process. If the treatment is mild, then the regimen remains the same, the treatment does not require changing living conditions, only the hygiene correction changes and the selection of medications is carried out.
Moderate condition is usually treated at home with bed rest. In case of severe cases, hospitalization in a hospital may be required.
Diet
As in the case of any inflammatory disease, a nutritious diet is prescribed, with a sufficient content of all necessary substances, including vitamins and minerals. But with vulvitis there are some peculiarities in nutrition.
It is necessary to use those products that cause a change in the body’s environment in the alkaline direction, avoid the use of products that cause acidification of the environment:
- The first group includes such products as dairy products, cereals, boiled meat and vegetable dishes.
- The second group , which is subject to restrictions, includes smoked, salted, fatty and refined products, which contain a large amount of harmful substances, as well as fatty broths or broths and spices of various types.
If vulvitis is of an allergic nature, then the diet is prescribed taking into account the pathogenic component that caused it, as well as other highly allergenic products (these are any citrus fruits, honey, cocoa-containing products).
Local treatment
The main part of local therapy is the use of antiseptic and anti-inflammatory solutions:
- For this purpose, they can be used as local herbal therapy , such as a decoction of oak bark, chamomile, calendula, and St. John's wort.
- As well as medicinal antiseptics. Furacilin solution , which is prepared by mixing a tablet or powder with water. Also potassium permanganate , which is dissolved in water and brought to a pale pink color. You can also use a ready-made solution of Chlorhexidine . The advantage of using it is its ease of preparation; all you need to do is buy a bottle of a solution of the required concentration. An analogue of this remedy is Miramistin .
- In advanced cases, antibacterial ointments are prescribed and applied to the vulva area. These most often include Tetracycline and Erythromycin . But tetracycline ointment has age restrictions, so it should not be prescribed to girls under 8 years of age.

Erythromycin ointment

Furacilin

Chlorhexidine

Miramistin

Potassium permanganate

Tetracycline ointment
Etiotropic therapy
Mainly in case of detection of a disease, especially in severe cases, before prescribing therapy, use the determination of sensitivity to antibacterial agents:
- If it is determined that the causative agent is a fungus , then treatment is reduced to the prescription of antifungal agents. This could be Fluconazole, Miconazole, Itraconazole, Levorin, etc. These drugs are prescribed systemically in tablet form.
- And as local therapy, agents such as Clotrimazole and Decamine ointment . With pre-treatment of the vulva with soda solution.
- The bacterial nature of vulvitis is treated by prescribing antibacterial agents such as Metronidazole or Ceftriaxone. A specific infection identified as a pathogen is transferred to a dermatovenerologist for treatment.

Clotrimazole

Fluconazole

Itraconazole

Miconazole

Ceftriaxone

Metronidazole
Hygiene
This is one of the fundamental rules in the treatment of inflammation of the vulva. In case of illness in girls at a young age, hygiene skills are taught to parents or caregivers.
But if these are older girls, then the doctor explains to her the basic recommendations regarding hygiene:
- The main thing everyone needs to remember is the correct movements. They should be carried out only in one direction, from the pubis to the anus. You should not make rubbing movements or rub this area with any hygiene products (rags, washcloths, brushes).
- It is better to perform all manipulations with clean hands. A single movement is required followed by rinsing the hand, thereby washing away the bacteria. The toilet of the genital organs must be carried out after each act of urination or defecation, and it is not always necessary to use specialized means.
- In most cases, it should be clean water, at a comfortable temperature , i.e. slightly warmed up. Under no circumstances should you use excessively hot or cold water.
- Specialized hygiene products are used no more than twice a day . It is better if they are appropriate for their age and purpose, avoiding purchasing scented or substances containing dyes. It is preferable to use products with a hypoallergenic composition, such as the Mustela and Weleda .
- It is recommended to use diapers as little as possible in everyday life , regardless of age. But if this is not possible, then during the day the diaper can be left for a maximum of three hours, after which a mandatory replacement is required, even if it turns out to be unused. And at night it is allowed to increase the time to 5-6 hours.
- At any age, girls need to follow the rules of wearing underwear . Its composition must be natural and not contain any admixtures of artificial components, especially those of synthetic origin. And also true to size, without chafing areas.
Air baths are also mandatory for girls. This does not require special skills or preparation; the girl, naked in the lower parts of the body, is simply placed on a dry and clean diaper in a room with a comfortable temperature. The minimum duration of one procedure should be a quarter of an hour.
Normalization of general condition with vulvitis
First of all, to alleviate general well-being, desensitization agents are prescribed. They help relieve symptoms such as itching, burning, and severe swelling. Can be used in both local and systemic form.
The use of such agents as immunostimulants, vitamins and interferon inducers is also indicated. In case of frequent relapses, hormonal agents based on estrogen begin to be used, since it is through them that the process of formation of a normal microbiocenosis occurs. In addition, subsequently, means are used to restore microbiocenosis based on lactobacilli.
Sanitation of foci of infection
This is one of the mandatory points in the treatment of pathology.
This is due to the fact that vulvitis is almost always provoked by another infection in the body. The most common among them may be the following:
- dental caries,
- inflammatory kidney diseases, often in the chronic stage,
- ORZ.
Therefore, first of all, it is necessary to identify and treat this pathology.
In addition, helminthic infestation can serve as a source of infection; enterobiasis is one of the most common causes. Therefore, the use of anthelmintic therapy is required. In very rare cases, a foreign body can serve as a source of chronic infection. Therefore, its safest removal is required.
Physiotherapy for vulvitis in girls
This method of treating vulvitis in girls is not the main one, but at the same time it can significantly complement medication.
There are several different options for this:
- With the help of UV irradiation it is possible to achieve permanent death of microorganisms.
- Electrophoresis method with drugs, for example, zinc. Used for fungal etiology.
- Ultrahigh-frequency effects are effective in cases of extensive local lesions. Able to reduce swelling, itching, capillary permeability.
- The effect of Darsonval currents on the vulva area has an antipruritic effect and also accelerates the death of fungi.
- Laser irradiation of blood as a method of therapy is used very rarely to treat vaginitis in girls. It is prescribed only in case of frequent relapses and severe course of the process.
A selection of effective treatment methods
Treatment of vulvitis in girls consists of a set of measures depending on the etiology of the infection.
Nutrition and regimen
In case of an acute process, girls need to be provided with bed rest. During illness, you should change your diet. Reduce the intake of foods that promote the formation of acids and spices (fried foods, meat broths, smoked foods, pickled vegetables, sour fruits). You need to increase alkalizing foods in your diet (milk, fresh and boiled vegetables). If vulvitis is of an allergic nature, a hypoallergenic diet is indicated. It involves eliminating allergenic foods from the diet:
- nuts;
- eggs;
- citrus;
- chocolate;
- honey.
After an acute period, to restore the microflora of the vagina and intestines, you can diversify the menu with fermented milk products.
Local therapy
It is indicated for the elimination of hyperemia and swelling of the genital organs, relieving the unpleasant symptoms of burning and itching. For this purpose, disinfectants are used in the form of baths, irrigations, and lotions.
Local antiseptics:
- Potassium permanganate solution (light pink);
- Chlorhexidine;
- Miramistin;
- Furacilin;
- Quinozol.
Herbal infusions:
- calendula;
- chamomile;
- sage;
- nettle;
- series;
- oak bark
Find out about exercises to correct dyslexia in primary schoolchildren.
How to get rid of lamblia in a child? Treatment methods are described in this article.
At the address, read the instructions for using Ambrobene solution for inhalation.
Effectively treat inflamed areas with ointments:
- Tetracycline (after 8 years);
- Oletetrinovaya;
- Sangiviritin 1%;
- Erythromycin.
The ointment should be applied carefully to previously washed and dry genitals. Long-term use of ointments is not recommended. If the inflammation does not go away, you need to show the child to a doctor to adjust the treatment.
READ ALSO: Viral skin disease - molluscum contagiosum in children: photos of papules, routes of transmission and infection, methods of treating the disease
If the disease is recurrent, estrogens (Folliculin, Estriol) are applied topically to accelerate reparative processes.
Systemic treatment
When the nature of vulvitis and its causative agent are determined, the doctor can prescribe medications for oral use.
Candidiasis vulvitis is treated with antimycotic agents:
- Levorin;
- Fluconazole;
- Itraconazole
In parallel, areas of inflammation are treated locally with antifungal ointments (Clotrimazole, Decamine ointment).
If trichomonas are detected within 7-10 days, the following are prescribed:
- Metronidazole;
- Tinidazole;
- Ornidazole.
For prolonged trichomonas vulvitis with relapses, Solcotrichovac is administered intramuscularly (3 injections of ½ ml every 14 days). A second injection is carried out after a year - ½ ml once.
Gonococcal infection is treated with cephalosporin antibiotics:
- Cefatoxime;
- Cefix;
- Ceftriaxone.
In the presence of chlamydia and mycoplasmas, broad-spectrum antibiotics are prescribed:
- Sumamed;
- Doxycycline.
Vulvitis against the background of helminthic infestations begins to be treated with anthelmintic drugs:
- Wormil;
- Pyrantel;
- Levamisole;
- Albendazole.
Normalization of general condition
In case of vulvitis, it is necessary to take desensitizing agents to relieve swelling and itching:
- Suprastin;
- Tavegil;
- Zyrtec.
Enzymatic agents to normalize digestion:
- Baktisubtil;
- Creon;
- Wobenzym.
Immunomodulators to increase the body's protective functions:
- Immunal;
- Immunoflazid.
Folk remedies and recipes
Traditional medicine methods can be highly effective in treating vulvitis in girls. Recipes:
- Infuse 1 spoon of St. John's wort in 200 ml of boiling water for 1 hour and strain. Take 50 ml orally three times a day.
- Pour 1 spoon of dried viburnum flowers into a glass of water. Leave in a water bath for 10 minutes. Filter and drink 1 spoon three times a day.
- To relieve itching and burning, externally use baths and washes with a decoction of chamomile or oak bark (2 spoons per 1 liter of water).
Traditional recipes for the treatment of vulvitis in girls
To treat vulvitis in girls at home, baths with decoctions of medicines are used.
The main ones include:
- Chamomile decoction , this remedy has been known for a very long time as an anti-inflammatory drug that can relieve not only swelling and inflammation, but also, to a small extent, itching. It is prepared by steaming several tablespoons of the plant in boiled water; some recommend boiling the mixture in water for a short time or simply leaving it in a container, covered with a towel. After which the mixture is filtered. The resulting solution is used as sitz baths, so the effect is much faster, but it should be noted that the water should be at a comfortable warm temperature; the decoction should not be too cold or hot.
- Calendula decoction. A product that has similar properties, but has certain advantages. More often used for people with a tendency to allergic diseases. It is prepared in the same way as the previous one; you can use either a self-prepared plant or a ready-made one purchased at a pharmacy. Also used as baths or lotions.
- Oak bark extract. Used as a sitz bath and has an anti-inflammatory effect. To do this, pour boiling water over the dry mixture and cook for several minutes, then cool and strain. The duration of the procedure can be up to 30 minutes.
- If a candida cause of inflammation is established, then soda solutions are used to relieve symptoms and reduce the pathogenic properties of the pathogen. More often used as lotions. To do this, you need to prepare a solution of baking soda by mixing a tablespoon with 1 liter of clean boiled warm water.
Treatment options for rashes on the labia in girls
Typical treatment for diaper rash involves keeping the girl's perineum and genitals as clean and dry as possible. You can also try:
- changing diapers if the existing ones quickly get wet or irritate;
- washing with a soft cloth with hypoallergenic agents;
- frequent ventilation of the perineum, walking without a diaper;
- applying a cream containing zinc oxide.
But if these treatments don't work, your doctor may prescribe special anti-inflammatory ointments. He will examine the area to determine whether the lesion is fungal or bacterial in nature. If necessary, he may take a skin sample to determine the exact cause.
Examples of treatments that may help relieve persistent diaper rash include:
- hydrocortisone cream
- antifungal cream
- local antibiotics.
If the infection is bacterial, your doctor may also prescribe oral antibiotics.
Important
Parents should never use over-the-counter hydrocortisone or antibiotics to treat their child without the advice of a doctor. You should also avoid products that may be harmful or potentially toxic to children, including ingredients such as benzocaine, camphor, and salicylates. Using medicated ointments that are not suitable for a girl's skin can do more harm than help.
Home treatments
Parents can independently cope with skin irritation or sweating, rashes on the girl’s genitals, using some useful recommendations:
- Airing the baby's skin. It is necessary to schedule several periods during the day when the girl will not wear a diaper to allow the skin to ventilate and remain dry. You can place your baby on a waterproof or washable changing mat for 10 minutes to give the skin more air.
- Changing diaper size. Diapers that are too tight can hold moisture closer to the skin. By temporarily increasing the diaper size, you can reduce irritation and wetness, eliminating existing genital rashes. It's also worth changing your diaper for nighttime use so it absorbs more moisture.
When to see a doctor
You should see a doctor if your child's rash does not go away or improve after a few days of home care. Some other signs that a diaper rash should be examined by a specialist include:
- bleeding, oozing sores on the perineum or itchy skin;
- fever due to rash;
- pain every time you urinate or have a bowel movement.
In this case, an accurate diagnosis and treatment tactics are needed to prevent complications.
Alena Paretskaya, pediatrician, medical columnist
2, total, today
( 53 votes, average: 4.40 out of 5)
Cervicitis of the cervix: causes, symptoms, treatment
Hysterectomy, or removal of the uterus: indications and consequences
Related Posts
Complications of vulvitis in girls
They arise against the background of a long-term inflammatory process without adequate and timely treatment.
These include the following conditions:
- Fusion in the area of the labia minora . This occurs due to the gradual development of synechia, against the background of fibrin deposits during vulvitis in girls.
- Adhesions in the vaginal area. They are the result of the transition of the inflammatory process to the overlying sections in severe vulvitis. Subsequently, they lead to problems in sexual life, and can also indirectly complicate the process of labor, leading to the appearance of gaps.
- Involvement of other systems and organs in the inflammatory process. So, due to the close anatomical location, acute cystitis or proctitis, as well as cracks in the anal area, can occur.
- The appearance of scar changes at the site of former vulvitis in girls , which subsequently causes complexes and discomfort.
- Change in skin color . As a result, the external genitalia become bluish and persist for a long time or even for life.
Genital thrush in children
- 1 Why does it occur?
- 2 Symptoms of thrush in children on the genital area
- 3 Treatment of candidiasis 3.1 Medication
- 3.2 Folk remedies
Have you been trying to cure FUNGUS for many years?
Head of the Institute: “You will be amazed at how easy it is to cure fungus by taking the product every day for 147 rubles ...
Read more "
Genital thrush in children is common. This disease provokes the proliferation of the Candida fungus. This disease is difficult for children to tolerate. To complicate the situation, they can reinfect themselves if they are not monitored. This significantly prolongs therapy. Sometimes thrush becomes chronic; to prevent this from happening, consult a doctor.

Why does it happen?
A child can only become infected from an adult.
Most often, thrush in children in the groin area occurs at a young age. Thrush in newborns can be transmitted from the mother during childbirth. The baby's immune system is not yet strong enough to fight this disease. Candidiasis in children under one year of age is also transmitted through mother's milk. This disease also occurs in older children. In this case, the fungus is transmitted if children's clothes are washed with adults' clothes, through unwashed food and dirty hands. In addition, this disease can be caused by a disorder of carbohydrate metabolism.
Return to contents
Symptoms of thrush in children on the genital area
Inflamed areas of the genitals cause burning and itching.
Genital thrush in boys is visible to the naked eye. A white, cheesy coating forms on the weenie, which cannot be erased. Ulcers form on the pussy. The foreskin becomes inflamed. Thrush in girls also forms plaque on the labia. The baby's temperature rises to 37.5 C. The child experiences burning and itching. He is restless and does not sleep well. The greatest discomfort is caused by urination. Thrush looks unpleasant.
Return to contents
Treatment of candidiasis
As in adults, treatment depends on the stage and state of the immune system. Thrush can be treated in 2 ways:
- medicines;
- traditional medicine.
In addition, treatment will be effective if you adhere to a diet. It is important to remove foods from your diet that promote Candida growth. These include:
- sugar;
- fruits;
- baked goods (anything that contains yeast).
Return to contents
Medication
Treatment for a newborn girl is difficult, since suppositories need to be inserted into the vagina. This is very inconvenient and experts advise using ointments. They are easy to smear on the labia for thrush in girls and pussy in boys. The most popular drugs are discussed in the table:
| A drug | Application |
| For babies | |
| Zelenka | 5 drops of brilliant green are diluted with a teaspoon of peroxide and water. Good for treating groin problems. Apply once a day after a bath. |
| "Holisal" | The gel is applied with a cotton swab several times a day. |
| "Levorin" | The tablets are ground and diluted in vitamin B12 to form a suspension. |
| For children over 6 months | |
| "Miramistin" | Available in the form of a solution and ointment. Apply a small layer with a cotton swab. |
| "Candide" | Apply with a cotton swab to the mucous membranes no more than 4 times a day. |
| Patients per year | |
| "Diflucan" | At this age, thrush is very rare. The ointment is applied with a cotton pad in a thin layer 2-3 times a day. |
The local action of the ointment makes its use safer.
Pensioners! Don't cut fungal nails! They are derived simply: take 9 grams...
Military doctor: So that the soldiers do not have fungus, they 2 times a day...
All drugs that are suitable for young children are used by children and older children. Starting from 3 years old, you can use drugs that are allowed for adults (“Pimafucin”). The use of any medication is discussed with a doctor. A girl’s thrush goes away in 7 days, the symptoms subside in 2-3 days. However, you should not stop treatment. This leads to a quick relapse.
Return to contents
Folk remedies
Traditional medicine cannot completely eliminate the disease. It is used as an adjuvant therapy to medication.
The genital organs of a child are most susceptible to damage. Folk remedies to cure the disease are described in the table:
| Way | Application |
| Calendula decoction | 2 tablespoons of flowers are poured with half a liter of boiling water. The genitals are washed, and girls are douched. |
| Aloe | The juice is applied to the plaque on the head. |
| Herbal mixture | A decoction is made from sage, plantain, thyme and chamomile. They wash it off. |
Prevention of vulvitis in girls
It comes down to the basic rules that must be included in the lifestyle:
- This is proper and complete nutrition.
- Sanitation of foci of chronic infection. Relieving the manifestations of allergic reactions, eliminating contact with the allergen.
- Regular hygiene procedures , use of correct and clean clothes. Avoiding wearing things that are too tight and that rub, in order to prevent the occurrence of illness.
- Avoid uncontrolled use of medications , mainly antibacterial ones.
- Timely contact a specialist when the first signs of an inflammatory process appear.