Hypotrophy in children is starvation, quantitative or qualitative, as a result of which significant changes occur in the body. Qualitative fasting is possible due to improper artificial feeding, lack of essential nutrients and vitamins, quantitative fasting - due to incorrect calculation of calorie content or lack of food resources.
Hypotrophy can be a consequence of acute diseases or the result of a chronic inflammatory process. Wrong actions of parents - lack of routine, poor care, unsanitary conditions, lack of fresh air - also lead to this condition.
What does a baby who is developing normally look like?
Signs of normotrophic:
- Healthy looking
- The skin is pink, velvety, elastic
- Lively look, active, exploring the world around him with interest
- Regular increase in weight and height
- Timely mental development
- Proper functioning of organs and systems
- High resistance to adverse environmental factors, including infectious ones
- Rarely cries
In medicine, this concept is used only in children under 2 years of age. According to WHO, malnutrition is not widespread:
- in developed countries its percentage is less than 10,
- and in developing countries – more than 20.
According to scientific research, this deficiency condition occurs approximately equally in both boys and girls. Severe cases of malnutrition are observed in 10-12 percent of cases, and in a fifth of children it is accompanied by rickets, and in a tenth by anemia. Half of the children with this pathology are born during the cold season.
Hypotrophy in children
The term malnutrition comes from two Greek words - hypo - lower, trophe - nutrition.
Reference! According to ongoing research, the deficiency state is observed with equal frequency in both boys and girls. It is noteworthy that half of the children with this diagnosis were born in the cold season.
From birth, the child begins to significantly gain body weight, all his organs are actively growing, and if the baby is not fed correctly, signs of malnutrition immediately appear. Most often, this pathology develops due to a lack of calories and proteins in the child’s diet. Initially, a lag in body weight manifests itself in disorders of the gastrointestinal tract, as a result of which the absorption of nutrients is impaired. In addition, the child may suffer from a lack of microelements and vitamins.
Causes and development
The causes of malnutrition in children are varied. The main factor causing intrauterine hypotrophy is toxicosis in the first and second half of pregnancy. Other causes of congenital malnutrition are:
- pregnancy before the age of 20 or after 40 years
- bad habits of the expectant mother, poor nutrition
- chronic diseases of the mother (endocrine pathologies, heart defects, etc.)
- chronic stress
- mother's work during pregnancy in hazardous work (noise, vibration, chemicals)
- pathology of the placenta (improper attachment, early aging, one umbilical artery instead of two and other disorders of the placental circulation)
- multiple pregnancy
- hereditary metabolic disorders in the fetus
- genetic mutations and intrauterine anomalies
Causes of acquired malnutrition
Internal - caused by pathologies of the body that disrupt food intake and digestion, absorption of nutrients and metabolism:
- congenital malformations
- CNS lesions
- immunodeficiency
- endocrine diseases
- metabolic disorders
In the group of endogenous factors, it is worth highlighting food allergies and three hereditary diseases that occur with malabsorption syndrome - one of the common causes of malnutrition in children:
- cystic fibrosis - a disorder of the exocrine glands, affecting the gastrointestinal tract and respiratory system
- celiac disease - gluten intolerance, changes in the functioning of the child’s intestines begin from the moment gluten-containing products are introduced into the diet - barley, semolina, wheat porridge, rye, oatmeal
- lactase deficiency - the digestibility of milk is impaired (lactase deficiency).
According to scientific research, malabsorption syndrome provokes malnutrition twice as often as nutritional deficiency. This syndrome is characterized primarily by impaired stool: it becomes copious, watery, frequent, and foamy.
External - caused by incorrect actions of parents and unfavorable environment:
| Nutritional factor | Insufficient supply of breast milk; incorrectly selected formula for artificial feeding; Complementary feeding was introduced late, a small amount of calories in complementary feeding, imbalance in proteins, fats and carbohydrates |
| Infectious factor | Intestinal infections; Chronic infections, frequent acute respiratory viral infections and other diseases |
| Toxic factor | Unfavorable environmental conditions, medication, poisoning, excessive intake of vitamins, especially A and D |
| Social factor | Inattentive attitude of parents towards the child, lack of walks in the fresh air, affection, care, communication with mother, lack of gymnastics and massage |
All exogenous factors in the development of malnutrition cause stress in the child. It has been proven that mild stress increases the need for energy by 20% and protein by 50-80%, moderate stress by 20-40% and 100-150%, severe stress by 40-70 and 150-200%, respectively.
Symptoms
Signs and symptoms of intrauterine hypotrophy in a child:
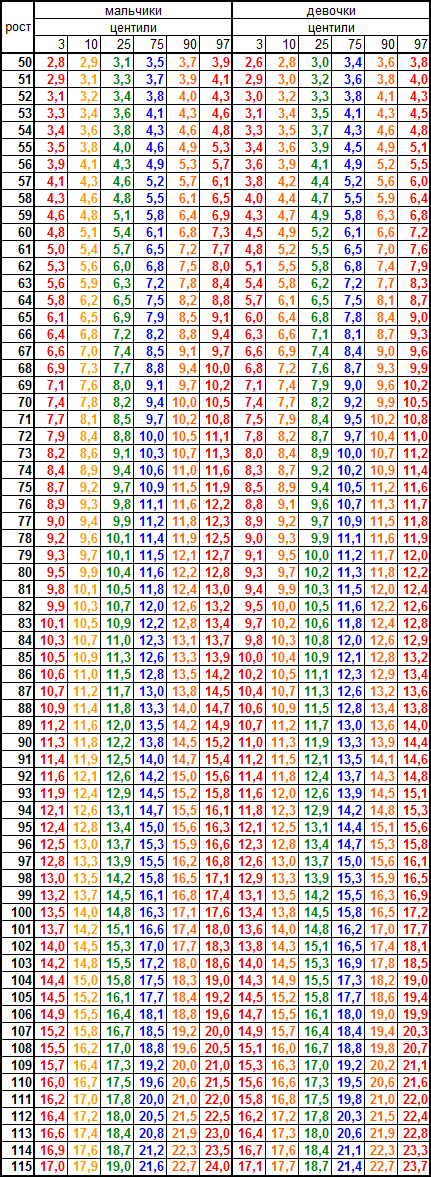
- body weight below normal by 15% or more (see below table of the relationship between weight and height of the child)
- height is 2-4 cm less
- the child is lethargic, muscle tone is reduced
- innate reflexes are weak
- thermoregulation is impaired - the child freezes or overheats faster and stronger than normal
- subsequently the original weight is slowly restored
- umbilical wound does not heal well
Acquired malnutrition is characterized by common features in the form of clinical syndromes.
- Lack of nutrition: the child is thin, but the body proportions are not impaired.
- Trophic disorders (malnutrition of body tissues): the subcutaneous fat layer is thinned (first on the abdomen, then on the limbs, in severe cases and on the face), the mass is insufficient, the body proportions are disturbed, the skin is dry, elasticity is reduced.
- Changes in the functioning of the nervous system: depressed mood, decreased muscle tone, weakened reflexes, psychomotor development is delayed, and in severe cases, acquired skills even disappear.
- Decreased perception of food: appetite worsens to the point of its complete absence, frequent regurgitation, vomiting, stool disorders appear, the secretion of digestive enzymes is inhibited.
- Decreased immunity: the child begins to get sick often, chronic infectious and inflammatory diseases develop, possibly toxic and bacterial damage to the blood, the body suffers from general dysbiosis.
Signs of 3rd degree malnutrition in children
This degree is considered severe, since all symptoms only worsen, and without timely treatment lead to death in children. In addition to all the above-described signs, there are signs of disruption of the activity of all organs and systems:
- Weight deficit is 30% or more.
- Growth retardation.
- Lack of subcutaneous fat.
- There are disturbances in heart rhythm and heart function.
- Breathing problems.
- Mental retardation.
- Muscle atrophy and skin folding.
- Symptoms of anorexia.
- Violation of thermoregulation and decreased blood pressure.
Treatment of this degree of malnutrition should be carried out only in a hospital, since the functioning of metabolic processes and the activity of all organs and systems are disrupted. Drug treatment includes intravenous transfusion of blood, plasma, glucose solution, hormones, as well as treatment with enzymes, vitamins, and microelement compounds.
Degrees of malnutrition in children
Hypotrophy of the first degree is sometimes almost invisible. Only an attentive doctor can identify it during an examination, and even then he will first conduct a differential diagnosis and find out whether an 11-20% body weight deficit is a feature of the child’s physique. Thin and tall children are usually so due to hereditary characteristics. Therefore, a young mother should not be alarmed if her active, cheerful, well-nourished child is not as well-fed as other children.
First degree hypotrophy in children is characterized by a slight decrease in appetite, anxiety, and sleep disturbances. The surface of the skin is practically unchanged, but its elasticity is reduced, and the appearance may be pale. The child looks thin only in the abdominal area. Muscle tone is normal or slightly decreased. Sometimes signs of rickets and anemia are found. Children get sick more often than their well-fed peers. Changes in stool are minor: tendency to constipation or vice versa.
Hypotrophy of the 2nd degree in children is manifested by a weight deficit of 20-30% and growth retardation (about 2-4 cm). The mother may notice that the child has cold hands and feet, he may burp frequently, refuse to eat, be lethargic, inactive, and sad. Such children are lagging behind in mental and motor development and sleep poorly. Their skin is dry, pale, flaky, wrinkles easily, and inelastic. The child appears thin in the abdomen and limbs, and the outline of the ribs is visible. Stool fluctuates greatly from constipation to diarrhea. Such children get sick every quarter.
Sometimes doctors see malnutrition even in a healthy child who looks too thin. But if the height corresponds to his age, he is active, mobile and happy, then the lack of subcutaneous fat is explained by the individual characteristics and high mobility of the baby.
With grade 3 malnutrition, growth retardation is 7-10 cm, weight loss ≥ 30%. The child is drowsy, indifferent, whiny, acquired skills are lost. The subcutaneous fat is thinned everywhere, pale gray, dry skin stretches over the baby’s bones. There is muscle atrophy, the limbs are cold. The eyes and lips are dry, there are cracks around the mouth. A child often develops a chronic infection in the form of pneumonia or pyelonephritis.
Degrees of malnutrition in children and symptoms of the disorder
First degree
The disease is characterized by a slight decrease in appetite, accompanied by sleep disturbances and frequent anxiety. The baby's skin usually remains virtually unchanged, but has reduced elasticity and a pale appearance. Thinness is visible only in the abdominal area, while muscle tone may be normal (sometimes slightly reduced).
In some cases, grade 1 malnutrition in young children may be accompanied by anemia or rickets. There is also a general decrease in the functioning of the immune system, which causes children to get sick more often and look less well-fed in comparison with their peers. Some children may experience digestive upset leading to diarrhea or constipation.
Often, degree 1 of the disorder remains practically invisible to parents, and only an experienced doctor can identify it through a thorough examination and diagnosis, during which he must find out whether the baby’s thinness is a feature of his physique and a hereditary factor.
Some children inherit tall height and thinness from their parents, so a slender young mother should not worry that her baby does not look as well-fed as the rest if he is active, cheerful and eats well.
Second degree
It is characterized by insufficient weight in children in the amount of 20-30%, as well as a baby’s growth retardation, on average by 3-4 cm. In this case, the baby may experience frequent regurgitation, lethargy, refusal to eat, low mobility, a constant state of sadness, and also lack of warmth of the arms and legs.
With grade 2 malnutrition, newborns experience developmental delays not only in motor but also mental development, poor sleep, pale and dry skin, and frequent peeling of the epidermis. A baby's skin is inelastic and wrinkles easily.
Thinness is very pronounced and affects not only the abdominal area, but also the limbs, while the contours of the baby’s ribs are clearly visible. Children with this form of disorder often get sick and have unstable stools.

Third degree
Children with this form of disorder are severely stunted, on average up to 10 cm, and have a weight deficit of more than 30%. The condition is characterized by severe weakness, an indifferent attitude on the part of the child to almost everything, tearfulness, drowsiness, as well as rapid loss of many acquired skills.
The thinning of subcutaneous fatty tissue is clearly expressed throughout the child’s body, severe muscle atrophy, dry skin, and cold extremities are observed. The skin color is pale with a grayish tint. The baby's lips and eyes are dry, and there are cracks around the mouth. Children often suffer from various infectious diseases of the kidneys, lungs and other organs, for example, pyelonephritis, pneumonia.
Diagnostics
| Clinical methods: | Laboratory methods: |
|
|
Differential diagnosis
As mentioned above, the doctor first needs to figure out whether malnutrition is an individual feature of the body. In this case, no changes in the functioning of the body will be observed. In other cases, it is necessary to carry out a differential diagnosis of the pathology that led to malnutrition: congenital defects, diseases of the gastrointestinal tract or endocrine system, damage to the central nervous system, infections.
Diagnosis of malnutrition in children
Diagnosis is based on anthropometry data (a method of measuring the human body and its parts): lack of body weight and slower growth rates relative to proper values.
A blood test reveals anemia, with grade 3 malnutrition - absolute lymphopenia (decreased lymphocytes), slowed ESR.
Biochemical examination reveals:
- hypoalbuminemia (decreased albumin, a substance that is an integral part of blood plasma);
- dysproteinemia (imbalance between blood protein fractions);
- hypoglycemia (decreased glucose concentration);
- hypocholesterolemia (low cholesterol);
- dyslipilemia (lipid balance disorder).
Urine analysis reveals leukocyturia, ketone bodies, and excess ammonia. In the coprogram there are signs of impaired intestinal digestion.

Treatment
The main directions of treatment of malnutrition in children are as follows:
- Identifying the cause of malnutrition and eliminating it
- Proper care: daily routine, walks (3 hours daily, if it’s ≥5˚ outside), gymnastics and professional massage, swimming in warm baths (38 degrees) in the evening
- Organization of proper nutrition, balanced in proteins, fats and carbohydrates, as well as vitamins and microelements (diet therapy)
- Drug treatment
Treatment of congenital malnutrition consists of maintaining a constant body temperature in the child and establishing breastfeeding.
Nutrition for children with malnutrition
Diet therapy for malnutrition is divided into three stages.
| Stage 1 – the so-called “rejuvenation” of the diet | that is, they use food products intended for younger children. The child is fed frequently (up to 10 times a day), the diet is calculated based on actual body weight, and a diary is kept to monitor food absorption. The stage lasts 2-14 days (depending on the degree of malnutrition). |
| Stage 2 – transitional | Medicinal mixtures are added to the diet, nutrition is optimized to the approximate norm (according to the weight that the child should have). |
| Stage 3 – period of enhanced nutrition | The calorie content of the diet increases to 200 kilocalories per day (with the norm being 110-115). Special high-protein mixtures are used. For celiac disease, gluten-containing foods are excluded, fats are limited, and buckwheat, rice, and corn are recommended for the diet. In case of lactase deficiency, remove milk and dishes prepared with milk from foods. Instead, they use fermented milk products and soy mixtures. For cystic fibrosis, a diet with high calorie content, food should be salted. |
Main directions of drug therapy
- Pancreatic enzyme replacement therapy; drugs that increase the secretion of gastric enzymes
- Use of immunomodulators
- Treatment of intestinal dysbiosis
- Vitamin therapy
- Symptomatic therapy: correction of individual disorders (iron deficiency, increased excitability, stimulant drugs)
- In severe forms of malnutrition - anabolic drugs - drugs that promote the formation of building protein in the body for muscles and internal organs.
Treatment of malnutrition requires an individual approach. It would be more correct to say that children are nursed rather than treated. Vaccinations for malnutrition of the 1st degree are carried out according to a general schedule, for malnutrition of the 2nd and 3rd degrees - on an individual basis.
Treatment of malnutrition in children
Treatment of intrauterine fetal hypotrophy consists of prescribing to a pregnant woman:
- antiplatelet therapy (aimed at normalizing microcirculation in the fetoplacental system);
- beta-mimetic drugs (dilate spasmodic uterine arteries, eliminate fetoplacental insufficiency);
- metabolic therapy (vitamins, nootropics);
- antispasmodics (dilate blood vessels, improve the flow of nutrients to the fetus).
Actovegin, a drug that improves the brain’s immunity to hypoxia and enhances compensatory capabilities, can achieve good results in prenatal hypotrophy.
As for the treatment of malnutrition in children, grade 1 pathology can be treated on an outpatient basis. If the lack of weight is more than 20-30%, planned hospitalization is indicated. The main activities are aimed at:
- correction of the reasons that caused retardation in growth and development;
- enhanced child nutrition;
- organizing proper care;
- elimination of existing metabolic disorders.
Diet therapy for malnutrition in young children includes two stages. First, the doctor clarifies whether the little patient tolerates food well, and then gradually increases the calorie content and volume of food, taking into account the physiological age norm. The child is fed often, in fractional portions. If his sucking/swallowing reflex is weakened, nutrients are administered through a tube.
Drug therapy for the treatment of childhood malnutrition includes:
- anabolic hormones;
- adaptogens;
- vitamins;
- enzymes.
If the child is in critical condition, an intravenous infusion of glucose, vitamins, saline solutions, and protein hydrolysates is performed.
Research into the causes and symptoms of malnutrition in children
In one of the somatic hospitals, 40 case histories of children diagnosed with hypertrophy (19 boys and 21 girls 1-3 years old) were analyzed. The conclusions were obtained as a result of the analysis of specially designed questionnaires: most often, children with malnutrition were born from a pregnancy that occurred with pathologies, with heredity for gastrointestinal pathologies and allergic diseases, with intrauterine growth retardation.
| Common causes of malnutrition in children: |
|
| By severity: |
|
| Concomitant pathology: |
|
| The main symptoms of malnutrition: |
|
| Laboratory data: |
|
Prevention of malnutrition in children
Prevention of both intrauterine and acquired malnutrition begins with the fight for the woman’s health and for maintaining long-term breastfeeding.
The following areas of prevention are tracking basic anthropometric indicators (height, weight), monitoring children’s nutrition.
An important point is the timely detection and treatment of childhood diseases, congenital and hereditary pathologies, proper child care, and prevention of the influence of external factors in the development of malnutrition.
Things to remember:
- Mother's milk is the best and irreplaceable food for a baby up to one year old.
- At 6 months, the menu should be expanded to include plant foods (see how to properly introduce complementary foods to a child). Also, do not switch your child to adult food too early. Weaning a child from breastfeeding before 6 months is a crime against the baby; if there are problems with lactation, the child does not have enough milk, you must first put it to the breast and only then supplement it.
- Diversity in nutrition does not mean different types of cereals and pasta throughout the day. A nutritious diet consists of a balanced combination of proteins (animal, vegetable), carbohydrates (complex and simple), fats (animal and vegetable), that is, the diet must include vegetables, fruits, meat, and dairy products.
- As for meat - after a year it must be present in the child’s diet - this is an irreplaceable product, there can be no talk of any vegetarianism, only meat contains compounds necessary for growth, they are not produced in the body in the quantities needed for growth. full development and health.
- Important!!! There are no safe medications “just” to reduce or increase a child’s appetite.
Causes of malnutrition in children
Hypotrophy can be caused by various factors of both the perinatal and postnatal stages of child development.
Intrauterine malnutrition may be associated with the following points:
- toxicosis;
- gestosis;
- fetoplacental insufficiency;
- premature birth;
- fetal hypoxia;
- intrauterine infection;
- mother's bad habits;
- stressful situations and frequent depression in the mother;
- insufficient nutrition of a woman during pregnancy;
- non-compliance with the daily routine during pregnancy;
- unfavorable environmental living conditions;
- work of the expectant mother in hazardous work;
- the mother has serious pathologies - diabetes mellitus, heart disease, nephropathy, hypertension, pyelonephritis.
Acquired malnutrition can be caused by:
- congenital, in particular chromosomal developmental abnormalities;
- enzymatic deficiency (lactose deficiency, malabsorption syndrome, celiac disease),
- diathesis;
- immunodeficiency state;
- unbalanced diet;
- regular malnutrition associated with pathologies of maternal breastfeeding;
- malnutrition due to low lactation or decreased volume of formula;
- strong and frequent regurgitation;
- maternal nutritional deficiency, as a result of which the milk composition becomes poor quality;
- presence of intestinal infection;
- severe pneumonia;
- frequent colds;
- tuberculosis;
- unsanitary living conditions for the baby and improper care for him - lack of walks in the fresh air, insufficient sleep, and so on.
It happens that there are several reasons for the development of malnutrition, then the pathology develops faster. Inadequate nutrition worsens the immune system, and this in turn makes it possible for frequent infectious diseases to occur, which provokes weight loss in the child and increases the manifestations of malnutrition.
Table of weight versus height in children under 4 years of age
Very strong deviations in a child’s weight do not occur due to decreased appetite or some individual characteristics of the body - this is usually due to an unrecognized disease or lack of adequate nutrition in the child. A monotonous diet, nutrition that does not meet age-related needs, leads to painful underweight. The child’s weight should be controlled not so much by age as by the baby’s height. Below is a table of the relationship between the height and weight of a baby (girls and boys) from birth to 4 years:
- The norm
is the gap between
the GREEN and BLUE numbers of the weight value (25-75 centiles). - Weight loss is between the YELLOW and GREEN numbers (10-25 centiles), but may be a variant of the norm or a slight tendency to decrease body weight in relation to height.
- Weight gain - between the BLUE and YELLOW numbers (75-90 centiles) is both normal and indicates a trend toward weight gain.
- Increased or decreased body weight - between the RED and YELLOW numbers indicates both low body weight (3-10th centile) and increased (90-97th centile). This may indicate both the presence of a disease and the characteristics of the child. Such indicators require a thorough diagnosis of the child.
- Painful decrease or increase in body weight - beyond the RED limit (>97 or <3 centile). A child with this weight needs to establish the cause of malnutrition or obesity and adjust nutrition and prescribe treatment, massage, etc., since this is a manifestation of some disease and dangerously inharmonious development of organs and body systems, reducing resistance to infections and negative environmental factors.
Author:
Selezneva Valentina Anatolyevna physician-therapist