Hip dysplasia is a widespread congenital pathology that is diagnosed more often in girls than in boys. Clinically, it is manifested by shortening of one leg relative to the other, and impaired hip abduction. Treatment is usually conservative with swaddling, physiotherapeutic and massage procedures, and wearing orthopedic devices. Only if these methods are ineffective is surgical treatment for hip dysplasia (HJ) in children.
General description of hip dysplasia in children
With dysplasia of the hip joint, its underdevelopment or increased mobility is noted, which is combined with insufficiency of connective tissues. The danger of the pathology lies in frequent subluxations and dislocations of the hip. Underdevelopment of the joint varies in severity - it can be gross violations or excessive mobility against the background of weakness of the ligamentous-tendon apparatus. In the absence of medical intervention, severe complications arise, therefore, in pediatric orthopedics, special attention is paid to the timely detection of hip dysplasia in newborns.
The pathology is characterized by a disturbance in the development of one of the hip joint sections. This leads to the loss of the ability of the acetabular labrum, articular capsule, and ligaments to hold the head of the femur in the anatomically correct position. As a result, it shifts outward and at the same time upward—subluxation occurs. And in the complete absence of contact of the femoral head with the acetabulum, dislocation occurs.
Pathogenesis
Hip dysplasia is caused by a deficiency of connective tissue caused by mutations of various genes in different combinations and exposure to adverse environmental factors. Characteristic anatomical manifestations of hip dysplasia are underdevelopment of the joint: hypoplasia and flattening of the acetabulum in a newborn, slow development of the femoral head, bursal-ligamentous and neuromuscular apparatus of the joint, which causes its increased mobility.
Deviation classification
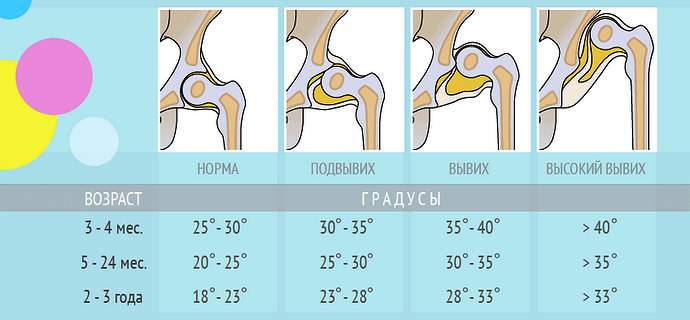
Hip dysplasia is classified depending on the severity of the resulting disturbances in its development. Dysplasia itself, or inferiority of the hip joint, is distinguished. This form of pathology does not manifest itself clinically, so it is difficult to diagnose it in a child only by external examination. Previously, it was not considered a disease, and its treatment was not carried out. Now it is impossible to do without therapy, as this can become a prerequisite for the development of complications. There are three degrees of severity of hip dysplasia:
- preluxation - a slight return displacement of the femoral head due to weakness of the joint capsule;
- subluxation - partial displacement of the head of the femur relative to the acetabulum with bending of the cartilaginous rim and tension of the ligaments;
- dislocation - complete displacement of the femoral head beyond the glenoid cavity.
The treatment tactics depend on the severity of hip joint underdevelopment. If special swaddling is sufficient for pre-dislocations, then for frequent dislocations surgical correction is often required.
| Form of hip dysplasia | Characteristics |
| Acetabular | The development of only the glenoid cavity is impaired. Its dimensions are smaller than anatomical, it is flattened, and the cartilaginous rim is underdeveloped |
| Femur | The angle of articulation of the femoral neck with its base is less or more than normal values |
| Rotary | The configuration of the articular structures in the horizontal plane is disturbed. The axes of movement of anatomical formations do not coincide during flexion and extension of the hip joint |
What is dysplasia in a child, what forms are there?
Hip dysplasia is a primary failure of the joint caused by a violation of its intrauterine development. Some authors believe that dysplasia in children under one year of age is a physiological phenomenon that, with adequate therapy, can be corrected without long-term consequences.
Knowledge of the anatomy of a newborn will help you understand what dysplasia is in a child.
A normal newborn joint consists of:
- femoral head;
- vetabular fossa, its depth is less than the diameter of the head;
- cartilaginous limbus or articular labrum - the formation is located along the edge of the cavity, increasing its depth and stabilizing the joint;
- periarticular capsule, tightly covering the joint and ensuring its stability;
- intra-articular and periarticular ligaments.
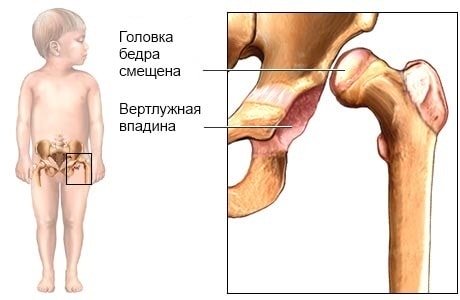
Localization of hip bones in a child with dysplasia.
A unique anatomical marker of a fully formed hip joint is the intraarticular ligament. Its role is to center the head in the cavity, especially in newborn babies, when the cavity is the most flattened and least consistent with the shape of the head.
The degree of underdevelopment of the baby’s hip joint is assessed by the number of signs of anomaly:
- the articular capsule is thin, stretched and the boundaries of its attachment are shifted;
- the external ligaments are underdeveloped and are not woven into the walls of the capsule;
- the ligament of the head of the femur is longer than the outer ones, has a ribbon-like shape, and is thin;
- the acetabulum is small, elongated, oval in shape;
- the articular labrum has uneven thickness, height, and is deformed;
- the head of the femur is larger than the socket, does not coincide with it in shape and is slightly deformed;
- The neck of the femur is thick, short, and poorly defined.
Depending on the number of detected deviations from the norm and identified developmental disorders and displacements, several forms of pathology are distinguished:
- preluxation;
- subluxation;
- dislocation.
In case of pre-luxation, the femoral joint is immature - 1-2 signs of dysplasia are noted, but the head is in the cotyloid cavity. Due to the stretched periarticular bursa and undeveloped ligament, the head moves easily, leaves the notch and also easily slides into it.
With subluxation, the joint is underdeveloped and the head is partially displaced relative to the center of the socket, but remains within the articular labrum, moving it upward.
Both forms are considered a conditionally normal variant of the structure of the hip joint. Under unfavorable conditions, preluxation and subluxation can lead to the most unfavorable variant of dysplasia - congenital dislocation.
In a dislocation, the proximal part of the bone is completely outside the glenoid cavity. You can imagine how severe a pathology congenital dislocation is and what the consequences of the lack of its correction are by seeing how a child with dysplasia walks and how his gait is changed.
One of the methods for correcting the consequences of hip dysplasia in girls
A girl is more at risk of the occurrence and development of pathology. Girls are 5 times more likely to have disorders. Most often, abnormal development is observed in the left joint (60%). The occurrence of aberrations in both joints or just the right one is the same.
Causes of the disease
The cause of hip dysplasia in children is a number of factors. Orthopedists especially highlight hereditary predisposition. If one of the parents was once diagnosed with congenital underdevelopment of the hip joint, then the likelihood of its occurrence in the child is 10 times higher.
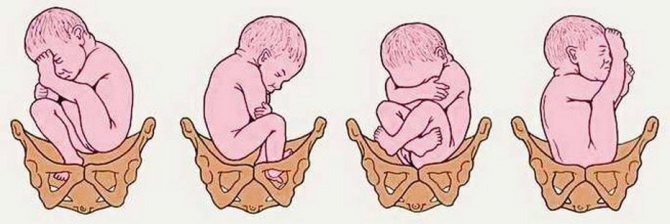
The risk of dysplasia increases significantly with breech presentation of the fetus - its longitudinal location in the uterus with the legs or buttocks facing the entrance to the pelvis. The following factors can provoke underdevelopment:
- severe toxicosis during pregnancy;
- the mother's intake of drugs from certain clinical and pharmacological groups, for example, glucocorticosteroids, immunosuppressants, cytostatics;
- large fruit;
- oligohydramnios;
- some gynecological pathologies that were untreated at the time of conception.
A relationship has been established between the frequency of births of children with hip joint underdevelopment and parents’ residence in an environmentally unfavorable region. Not least among the factors provoking acquired pathology is traditional tight swaddling.
Symptoms
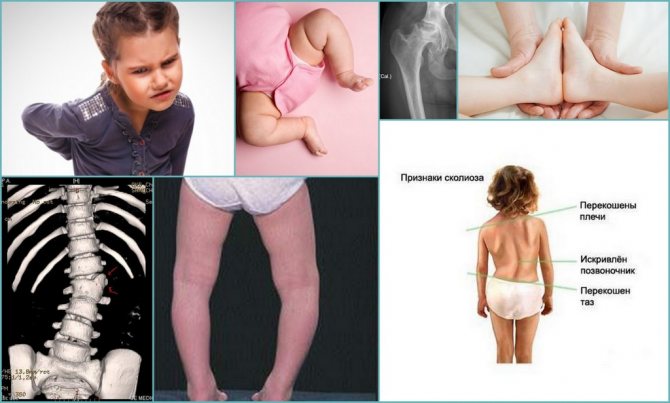
It is quite difficult to detect dysplasia at an early stage. The first clinical signs of pathology usually appear after 12 months. In newborns, the symptoms of dysplasia become easily distinguishable only when the disease is severe. So, the general signs of the disease include the following manifestations:
- Violation of hip abduction (i.e., legs bent at the knees are quite problematic to move apart). This symptom allows one to identify dysplasia in a baby in the first days after birth.
- Asymmetrical arrangement of skin folds in the buttocks and thighs. This symptom is diagnosed in a lying position (both on the back and on the stomach), and it is worth paying attention to the height and depth of the skin folds.
- A characteristic sound “click” when spreading the legs to the sides (while bending the knees). At the same time, a quiet crunching or clicking sound is heard.
- Shortening of one leg relative to the other. In this case, one knee will be located higher than the other (if you lay the baby on his back, bend his knees and place his feet on the table).
- Gait disturbance. The child may limp or walk on tiptoes without fully standing on the injured leg.
- Pain syndrome (usually occurs in severe cases of the disease). At the same time, the baby reacts with loud crying to any attempts to spread the half-bent legs to the sides.
There may also be excessive activity in the hip joints, i.e. the child will unnaturally turn his legs inward or outward.
Hip dysplasia in children under one year of age
Hip dysplasia in children under one year of age is determined by a pediatrician during examination. Children experience problematic hip abduction, and in advanced cases, shortening of the leg. Thus, the following signs serve as symptoms of pathology under the age of one year:
- asymmetry of skin folds on the legs;
- amyotrophy;
- “click” syndrome (see above);
- disturbance of the sucking reflex;
- pain and crying when trying to spread the bent legs to the sides.
We recommend: How to relieve a child’s cough?
But the symptoms of the disease may not be visible upon visual examination (if the initial stage of dysplasia occurs). An experienced pediatrician or pediatric orthopedist can make an accurate diagnosis.
Hip dysplasia in children after one year of age
If the disease is not identified in infancy and appropriate measures are not taken, dysplasia will subsequently cause many problems for the child and his parents. Obvious signs of pathology in children after one year include the following manifestations:
- pain and discomfort while walking (including due to inflammation of the joints);
- lameness;
- duck gait (occurs with bilateral dislocation).
Lack of timely treatment leads to serious undesirable consequences (death of the muscles of the diseased limb, dysfunction of the musculoskeletal system with subsequent disability, etc.).
Signs of pathology
Congenital underdevelopment of the hip joint can be diagnosed in the maternity hospital by a pediatric orthopedist based on its characteristic signs. He must also examine the child at the age of one, three, six and twelve months. Particular attention is paid to children without any symptoms of dysplasia, but who are at risk. These include newborns with a large weight or those who were in the breech position before birth.
In children older than one year, underdevelopment of the hip joint is indicated by gait disturbance (claudication), weakness of the gluteal muscles (Duchenne-Trendelenburg symptom), as well as higher localization of the greater trochanter.

Slipping symptom
The symptom of slipping (the “click” symptom, the Marx-Ortolani symptom) is detected only in children under 2-3 months of age in the supine position. When the doctor moves the child’s hip to the side evenly and gradually, a specific push is felt. Its appearance indicates the reduction of the head of the femur into the articular cavity, eliminating the condition of dislocation.
Lead limitation
This sign of dysplasia is detected in children under one year old in a supine position. The doctor bends the child's legs and then carefully spreads them to the side. With a correctly formed hip joint, the hip abduction angle is 80–90°. This symptom is not always informative. In healthy children, abduction limitation can be triggered by a physiological increase in muscle tone.

Leg shortening
This diagnostic sign allows us to identify the most severe form of hip joint - congenital dislocation. To do this, the child is placed on his back, and the doctor bends his legs, pressing him to his stomach. If dysplasia affects one hip joint, then the knee joints will not be located symmetrically due to shortening of the hip.
Symmetry of folds
With severe dysplasia, the inguinal, popliteal, and gluteal skin folds in a child older than 3 months are located asymmetrically. They also differ from each other in depth and shape. But such a symptom is informative only with unilateral damage. If two hip joints are underdeveloped at once, then the folds may well be located symmetrically. In addition, such a diagnostic sign is often absent in children with dysplasia and can be detected in a healthy child.
Diagnostics
To diagnose dysplasia, doctors conduct an examination and prescribe additional examinations. The choice of the appropriate examination method depends on the age of the child:
- Ultrasound examination of the hip joint - used most often in children under 4 months of age, before ossification of the femur occurs.
- X-ray is the main method for diagnosing hip dysplasia in children older than 4 months. It helps evaluate the shape of the acetabulum and femoral head and detect signs of arthritis, which sometimes appear in older children with hip dysplasia.
In teenagers, CT or MRI scans are sometimes done, which can provide more detailed images of the hip joints.

The neck-shaft angle characterizes the inclination of the femoral neck in the medial direction (in the vertical plane) from the longitudinal axis of the femur. In adults, the normal range is 125° – 135°. In children: newborns – 134°, 1 year – 148°, 3 years – 145°, 5 years – 142°, 9 years – 138°, in adolescence – 130°
Diagnosis of the disease
A doctor may suspect underdevelopment of the hip joint in a child immediately during his first external examination in his life. The examination is carried out after feeding, when the newborn is calm and relaxed. The primary diagnosis is made when one or more specific signs of dysplasia are detected, for example, limited hip abduction.
To confirm it, instrumental studies are prescribed, usually ultrasonography (ultrasound of the hip joint). X-rays are also used in diagnostics, but only in older children. The fact is that up to 3 months there is still a lot of cartilaginous tissue in the hip joint that is not visible on radiographic images.

First aid for hip dysplasia is to take your child to the doctor!
Even if you find all these symptoms in your baby, this does not mean that he is actually developing hip dysplasia. And vice versa - if you clearly do not detect any of these signs - this does not at all guarantee that the child does not have dysplasia. For example, underdevelopment of a joint can be bilateral. In this case, you will not find any asymmetry; as they say, things are equally bad on both fronts.
And therefore: the most reasonable solution (especially if you are at risk for joint dysplasia) is a preventive measure! That is: at the slightest doubt, go and show the baby to a pediatric orthopedist. In any case, he has something to check his suspicions - the presence or absence of hip dysplasia in children can be determined using medical procedures such as:
Ultrasound diagnostics. This is a screening test that is performed on all children aged 0 to 3 months. For older babies, as well as in case of remaining doubts, an x-ray is taken.
Radiography. Unfortunately, holding a tiny baby still while taking a photo is quite difficult. In addition, a baby’s bones are by no means as dense as those of adults, so they are much less visible in photographs. This means that when you go for an x-ray, you must “help” your orthopedist read the future image. For example, you can plan a trip to the X-ray room and the time your baby sleeps (if during the procedure he does not wake up and lies still, the picture will be much clearer and sharper).
How to properly treat a child
The sooner treatment begins, the faster the correct formation of the hip joint will be achieved. To do this, various methods and means are used to help fix the child’s legs in a position of flexion and abduction. This is a special wide swaddling blanket, stirrups, splints and other devices. The younger the child, the softer and more elastic the orthopedic products that support the legs should be.
Wide swaddling
This is more of a preventative measure rather than a curative one. Wide swaddling is recommended for parents of children who are at risk or who have been diagnosed with underdevelopment of the hip joint, which has not yet become the cause of pre-luxations, subluxations and dislocations. For the treatment of dysplasia, it is carried out only if it is impossible to use other, more effective methods of treatment.
To perform a wide swaddling, the baby is laid on his back, and two diapers are placed between his legs. They wrap loosely around each leg when flexed in abduction. The diapers are secured with a third, attached to the belt. This method of swaddling helps keep the legs apart at 60-80°.

Orthopedic structures
In the treatment of hip dysplasia in very young children, the Freik pillow is often used. Outwardly, it looks like a dense cushion located between the knees. And to secure the legs in a physiological position for the “ripening” of the hip joint, the design provides fixing straps.
Another frequently used device is Pavlik stirrups. This is the name of an orthopedic product that resembles a chest bandage. To securely fasten the legs, it is equipped with straps located on the child’s shoulders and behind the knees, ankle locks, and straps. Less commonly used is the Vilensky splint - two leather cuffs with a metal telescopic spacer between them.
Massage treatment
Restorative massage is an important component of therapy. The pediatric orthopedist writes out a referral for sessions. The massage is performed approximately an hour after the last feeding, in a calm, relaxing environment. It begins with stroking, light kneading and rubbing. Then the massage therapist begins more intense, energetic movements. This is necessary to strengthen the muscles of the thighs and legs and improve blood circulation. At the final stage, stroking is performed again.
Physiotherapy
Daily physical therapy exercises are necessarily indicated for dysplasia. A set of exercises is compiled by a pediatric orthopedist, taking into account the severity of the disease, the age of the child, and his general health. He shows parents how to perform the movements correctly to avoid excessive stress on the hip joint. What exercises are most effective:
- the legs are retracted to the sides, and then they perform circular movements with a small amplitude;
- when lying on your stomach, the legs are smoothly moved to the sides and then brought together;
- lying on the back, the legs are raised and the child's feet are brought together.
Regular exercise (up to 4 times a day) helps strengthen the muscles that support the head of the femur, preventing its displacement from the acetabulum. They also become an excellent prevention of the development of complications. Exercises are performed only as prescribed by a doctor, as there are contraindications to exercise, for example, an umbilical hernia.
Physiotherapy
To accelerate the “ripening” of the hip joint in its anatomical position, physiotherapy is used. Electrophoresis is prescribed with solutions of calcium, phosphorus, iodine - elements necessary for the proper formation of bone and cartilage structures. In total, about 10 sessions are performed, but if necessary, the course of treatment is extended.
UV irradiation of joints is also practiced according to a scheme determined individually. Thanks to the penetration of ultraviolet rays into the skin to a depth of 1 mm, local immunity is strengthened, metabolic and regenerative processes are accelerated.
Dysplasia is treated with applications of ozokerite or paraffin. These loose powders are preliminarily melted, cooled and applied layer by layer to the TBS. A thick film forms on the surface of the skin, retaining heat for a long time.
Surgical intervention
Indications for surgical intervention include severe hip dysplasia, detected at the age of 24 months, and the presence of anatomical defects in which it is impossible to reduce the dislocation. Surgeries are performed when the joint capsule is pinched, underdevelopment of the pelvic bones or hip bones. If it is impossible to reduce the head of the femur using a closed method, then surgical intervention is also used. What operations are performed for dysplasia:
- open reduction of dislocation - reduction of the femoral head into the acetabulum after dissection of the articular capsule, followed by casting for 3 weeks;
- surgery on the femoral bone - giving the proximal end of the femur the correct configuration using osteotomy;
- surgery on the pelvic bones - creating a support for the head of the femur, preventing it from slipping out of the socket.
If for some reason it is impossible to correct the configuration of the hip joint, then palliative operations are performed. Their goals are to improve the child’s well-being and restore some functions of the hip joint.
Treatment methods
A severe form of deviation is observed extremely rarely. Leg dysplasia in children can be eliminated in different ways: about 50 methods are known. All of them can be combined into three groups: medication, physiotherapy and surgery. The treatment plan is drawn up by the orthopedist after examining and examining the child.
Effective methods of treating leg dysplasia in children:
- loose or wide swaddling . The child's lower limbs are fixed in a slightly apart position. This method of wrapping allows you to prevent the onset of the disease and its progression. For wide swaddling, Becker pants are used;
- physiotherapy . Effective at the initial stages of pathology development. To achieve a positive result, you need to perform the exercises daily for 15-20 minutes. Gymnastics can be performed by a nurse in a children's clinic or by a mother at home;
- use of tires, stirrups, cushions, etc. Various technical means allow you to fix the child’s legs in the desired position. Vilensky and Volkov dividing tires are often used;
- massage . Prescribed to all children with leg dysplasia. It is important that manual therapy is carried out by a specialist who has experience working with children. During the massage, the effect is on the neck, back, hip joints;
- mud therapy . It is carried out in health centers, sanatoriums or the physiotherapy room of a children's clinic. Mud rich in minerals and other useful components is used that warms and heals joints;
- electrophoresis . Allows you to improve blood supply to cartilage tissue and reduce pain. The number of sessions and their frequency are determined by the doctor. Typically, about 2-3 courses are required per year;
- inducto- or thermotherapy . Such physiotherapy procedures are used for mild to moderate dysplasia. They are especially effective after surgical treatment: they eliminate unpleasant symptoms.
The operation is performed in severe cases when other methods do not give a positive result. Frequent relapses of the disease are also an indication for surgery. This method is used for children over one year old.
What are the complications?
In the absence of medical intervention, hip dysplasia becomes the cause of the development of numerous complications. The functional activity of one or two hip joints is reduced, which leads to disruption of the entire musculoskeletal system.
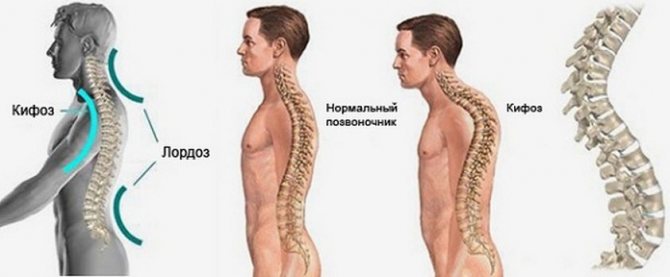
Disorders of the spinal column and lower extremities
Hip dysplasia provokes impaired motor skills of the spine, large and small joints of the legs. As the child grows up, gait becomes impaired due to developed flat feet, and scoliosis occurs—a persistent sideways curvature of the spinal column relative to its axis. This leads to an uneven distribution of loads on the vertebral structures during movement and the appearance of characteristic signs of osteochondrosis.
Dysplastic coxarthrosis
This is the name of severe degenerative-dystrophic pathology of the hip joint, which occurs due to the destruction of cartilage tissue with further deformation of the bones. In patients with dysplasia, the hip joints are formed incorrectly; under the influence of certain factors, the cartilage lining begins to thin out. After 25 years, dysplastic coxarthrosis can be triggered by low physical activity, excessive stress on the hip joint, changes in hormonal levels, and even taking drugs of certain clinical and pharmacological groups, for example, glucocorticosteroids.
Neoarthrosis
Neoarthrosis is a condition characterized by the formation of a false hip joint. With long-term dislocation, the femoral head flattens and the size of the acetabulum decreases. Where the head rests on the femur bone, a new joint gradually begins to form. Some doctors even consider this as self-healing, since the formed hip joint is capable of performing certain functions.
Aseptic necrosis of the femoral head
This pathology develops as a result of damage to the vessels supplying the head of the femur with nutrients. Aseptic necrosis in most cases occurs after surgery on the hip joint, including for the treatment of dysplasia. The femoral head begins to collapse, making independent movement impossible.
Causes
In the etiology of hip dysplasia in children, the leading role is played by the delayed development of the joint during intrauterine development (embryonic anlage), which develops under the influence of unfavorable endo/exofactors, as well as external influences on the joint after the birth of the child. Factors contributing to the development of hip dysplasia include:
- Unfavorable heredity (transmitted in an autosomal dominant manner from parents to child).
- Complications and unfavorable course of pregnancy (breech presentation of the fetus, large fetus, oligohydramnios, toxicosis of the first half of pregnancy, childbirth in women under 18 and over 35 years of age).
- Increased production of relaxin hormone , which is secreted in a woman’s body by the tissues of the uterus and placenta to prepare directly for childbirth (affects the ligaments, increasing their elasticity).
- Thyroid diseases.
- Infectious diseases from 10 to 15 weeks of pregnancy ( ARVI , rubella , influenza ).
- External influences - uncontrolled use of medications during pregnancy and alcohol, x-rays, radiation, unfavorable environmental conditions.
- Poor nutrition during pregnancy, contributing to the development of disorders of water-salt and protein metabolism, deficiency of vitamins and minerals in the body.
- Tight swaddling of the baby with straightened legs.
Prevention of DTS
The best way to prevent hip dysplasia is regular examination of the child by a pediatric orthopedist. Even if at some stage problems with the functioning of the hip joint are detected, timely treatment will allow you to completely get rid of the pathology.
Doctors strongly recommend that parents do not use tight swaddling, and often carry the child on his side in the “rider” position. In this position, he tightly clasps his mother or father with his legs, which contributes to the correct formation of the joints.
Prevention
Prevention of hip dysplasia in infants:
- Regular examination by a pediatric orthopedic specialist (at first, then every 3 months to a year).
- Performing a set of exercises designed to strengthen ligaments and muscles.
To prevent the development of dysplasia, you should not tightly swaddle a baby with straightened legs. With this position of the legs, even minor changes can turn into a full-fledged pathology.
Prognosis and complications
If treatment is not started immediately after the baby is diagnosed, then as the child grows older, when the child begins to stand on his feet, the load on the joint will be distributed incorrectly. In severe cases, joint dislocation occurs, even if the baby initially had an initial degree of dysplasia.
In this case, surgical intervention will be required to improve the patient's condition and regain mobility of the joint. The joint will no longer be completely healthy.
Interesting!
Some experts believe that about 50% of adults who experience osteoarthritis have suffered from undiagnosed hip dysplasia since childhood.
Lack of treatment for hip dysplasia in infants is dangerous; the following complications may occur:
- Scoliosis;
- Flat feet;
- Necrosis of the femoral head tissue;
- Osteochondrosis;
- Pathologies of the spine, legs and pelvis that interfere with the normal functioning of the musculoskeletal system.
Symptoms of untreated dysplasia
Treatment of hip dysplasia in babies under 3 months is the most effective, with more than 90% of cases of complete restoration of joint function. If therapy is started after six months, the chances of recovery become much lower.
Symptoms and severity
The first examination is carried out within the walls of the maternity hospital, immediately after birth . If dysplasia was diagnosed during this period, it will be easier to cope with underdevelopment of the femoral area. Sometimes symptoms of hip dysplasia in children can be noticed already at home, after discharge from the hospital (read about the symptoms of rickets in infants). Parents should be alert to the following manifestations:
- asymmetrical folds (gluteal, inguinal, femoral): if you put the baby on a flat surface, for example, on a changing table, and the legs are at the knees, all the inguinal, femoral and buttock folds will not be at the same level;
- different amplitude: if you put the baby on his back, bend his knees, and then straighten them to the sides, the knees will not touch the surface or will have a different angle of inclination.
All symptoms of a condition such as hip dysplasia in infants can be classified according to severity:
- 1st degree (pre-dislocation): the femoral part is underdeveloped, but there is no displacement of the femoral head;
- 2nd degree (subluxation): the head of the hip bone is partially displaced;
- 3rd degree (dislocation): the head is completely displaced.
. Follow the link to find out whether a hematoma on the head of a newborn is dangerous and how to determine its presence.
Causes and factors contributing to the development of pathology
What is hip dysplasia and what are the causes of the pathology? An incorrectly formed hip joint is a consequence of impaired development of the fetus during the intrauterine period , the formation of the musculoskeletal system starting from the 4-5th week of its stay in this environment.

Dysplasia causes the femoral head and acetabulum to misalign
Sources that can negatively affect the fetus include:
- gene mutations, which contribute to the development of orthopedic abnormalities with disruption of the primary anlage and the formation of a defect in the hip region of the embryo;
- negative physical and chemical agents that affect the fetus: ionization, chemicals, poisons, drugs that are abused by a woman during pregnancy;
- breech presentation of the fetus or large size of the fetus, which can cause displacement of the joints due to a violation of the anatomical localization of the fetus in the uterine environment;
- impaired water-salt metabolism in the fetus with the development of intrauterine infection or renal pathology.

Among the factors that relate to a pregnant woman are:
- development of a severe somatic illness in a pregnant woman: cardiac dysfunction, vascular pathology, severe renal or hepatic pathology, heart defect;
- development of vitamin deficiency, anemia;
- disrupted metabolic processes in a woman’s body;
- development of severe infectious and viral disease;
- maintaining an unhealthy lifestyle (abuse of smoking or drugs, alcohol), failure to maintain proper nutrition;
- early or late toxicosis.
There is a risk group for the development of this pathological condition, taking into account which a doctor can promptly identify hip dysplasia in children under one year of age. This group includes premature babies, large children, as well as children who were in the breech position in the womb. They take into account how complicated the medical history is and how the pregnancy proceeded.
Please note: if the child has too weak muscle tone, this may indicate hypotonia in the infant. This disease manifests itself in the inability of muscles to function normally.