Infectious agents
Many people believe that meningitis is a disease caused by a specific pathogen. This is far from true. The causative agents of the disease are numerous pathogenic agents. The most common pathologies in children aged two months and older are caused by the following viruses and bacteria:
- Neisseria meningitidis;
- Listeria monocytogenes;
- Streptococcus pneumoniae;
- Haemophilus influenzae.
When it comes to newborns, meningitis is caused by microorganisms such as Streptococcus agalactiae and Escherichia coli. In addition, in patients with congenital or acquired brain injuries, staphylococcal infection, anaerobic bacteria, and polymicrobial flora are often detected.
Causes of the disease
If we talk about the pathogenesis of the disease, it should be noted that the causative agents of meningitis can enter the brain area and directly into the subarachnoid space in various ways. More often than not, it is not possible to accurately diagnose the route of entry of the pathogenic agent.
With bacterial meningitis, the pathogen enters the brain in two ways. Primary bacterial meningitis occurs due to the entry of pathogenic bacteria directly from the mucous membrane to the brain tissue. Secondary - spread of infection from nearby foci, for example, from the area of ENT organs or from distant areas, such as the lungs and some others.
Viruses, fungi and bacteria enter the subarachnoid space through the blood and lymph. It is in this area of the brain that there is no cellular and humoral protection against pathogenic microorganisms. In addition, pathogenic microorganisms multiply well in this environment, because there are constant conditions of humidity, temperature and the availability of nutrients. Reproduction of pathogenic microflora occurs until the moment of phagocytosis. As a result of complex reactions in which microglial cells take part, the body’s reaction is triggered in the form of the development of an inflammatory process. After this, the patient develops a number of clinical signs that make it possible to diagnose meningitis.
Causes and symptoms
The initial sign of the development of a dangerous disease is a rash.
It can appear in the following places:
- sides;
- hips;
- shin;
- Feet;
- knees;
- forearms and hands;
- in rare cases on the face.
The rash appears due to pathogenic bacteria and viruses They cause an inflammatory process in the meninges, and this, in turn, affects the blood vessels. In particular, the capillary membranes are affected.
All this leads to the formation of local hemorrhage. This type of rash is commonly called hemorrhagic. In most cases, it makes itself felt with bacterial meningitis.
Reference! With the viral type of meningitis, immediate damage to the vascular endothelium occurs, which leads to a rash on the baby’s body.
By the way, not all parents pay attention to this symptom. Patients are admitted to the hospital already at the stage when a severe headache makes itself felt, body temperature rises, and frequent vomiting is present.
With meningitis, the rash is called erythema due to its characteristic appearance. Their appearance is explained by the fact that meningococcal toxin blocks blood vessels and increases the permeability of their walls.
Routes of infection
Parents often ask how meningitis is transmitted and why it happens? In fact, it is not meningitis that is transmitted, but the microorganisms that provoke it. If we consider the question of whether this pathology is contagious, the answer will be clearly positive. You can get sick through contact with an infected person.
Due to the fact that the causative agents of meningitis are viruses, bacteria or fungi, the routes of transmission can be as follows:
- airborne;
- contact and household;
- oral-fecal;
- from mother to child during childbirth, if the woman was infected during pregnancy
- through poorly washed vegetables and fruits;
- through water and dirty hands.
You can protect your child by practicing good hygiene and by keeping the patient away from the infected person.
What is the pathogenesis of its appearance?
The entry point for infection can be:
- upper respiratory tract (the pathogen enters the air through contact with a sick person or carrier);
- biological fluids of the body (the so-called parenteral transmission mechanism, when the pathogen enters the body when the integrity of the skin is damaged).
The contact and household mechanism of transmission is also discussed, as a result of which one can become infected through the immediate use of household items of the patient. Cases of infection of newborns from carrier mothers during passage through the birth canal have been described .
The etiological factor may be meningococcus, coliform bacteria, pseudomonas aerogenosis, enterococcus and other bacteria. Meningococcal meningitis is especially dangerous, the course of which often has a fulminant form and is called meningococcemia.
Viral pathogens: adenoviruses, enteroviruses, herpes virus and others.
Once in the human blood, the microorganism with its current reaches the cells of the brain membrane, penetrates them and begins to destroy their structure. It is also capable of producing an aggressive toxin, which increases the permeability of the walls of blood vessels and provokes the release of blood under the skin.

Reversibility of such a process is possible only with emergency use of drugs that will deprive the pathogen of viability and maximally destroy its amount in the blood.
Types of meningitis
Doctors distinguish several types of pathology. Depending on the etiology, infectious, infectious-allergic, fungal, neuroviral, traumatic and microbial types of pathology are distinguished. Microbial meningitis is divided into influenza, serous, tuberculous and herpetic. In addition, the disease is classified depending on the location:
- pachymeningitis – damage to the hard membranes of the brain;
- leptomeningitis – damage to the soft and arachnoid membranes of the brain;
- panmeningitis - damage to all membranes of the organ.
It is worth noting that with the development of the inflammatory process due to damage by pathogenic microflora in the area of the arachnoid space, the pathology is classified into a separate group. Moreover, it is called arachnoiditis.
Depending on the origin, the pathology is divided into primary meningitis (neuroviral forms of the disease) and secondary (due to syphilis, tuberculosis, serous and other infections). If we take into account the nature of the fluid circulating in the ventricles of the brain (CSF), meningitis is divided into purulent, serous, hemorrhagic and mixed types.
All types of the disease have a similar clinical picture. The patient has an increase in intracranial pressure and a severe headache of a bursting nature. A person feels strong pressure in the ears, temples and eyes. The reaction to sounds and light increases significantly, and rashes, vomiting, and increased body temperature often occur.
You should go to the hospital without waiting for dangerous symptoms to develop. A quick response to the problem will help save the baby’s life and prevent serious consequences.
Symptoms of meningococcal meningitis
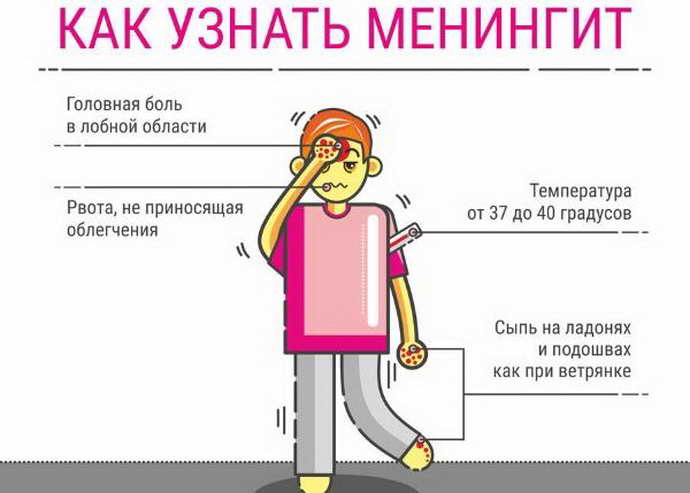
The causative agent of this type of pathology in children is meningococcus. In this case, the onset of meningitis is acute, and the patient experiences meningeal and cerebral symptoms. Among them the following should be highlighted:
- a sharp increase in body temperature to 39-40 degrees;
- body aches, severe pain in the head;
- painful sensations when moving the eyes;
- dizziness, nausea;
- “fountain” vomiting, which does not lead to relief;
- thirst.
You might be interested in: Whooping cough in children: symptoms, treatment, prevention and photos
Meningococcal infection in children causes an increased reaction to stimuli such as touch, sound, and light.

The patient shudders, which indicates the body's convulsive readiness. If we talk about children under one year old, it is worth emphasizing that they have convulsions - this is the first sign of developing meningitis. If convulsions occur in older children, then we are talking about a severe course of the disease, which requires immediate hospitalization. After 8-12 hours, the child develops meningeal syndrome. In this case, rigidity of the muscles of the occipital region occurs, as well as symptoms of irritation of the meninges (Kernig's symptoms) and Brudzinski's signs. In severe cases, paresis develops, reflexes are reduced or absent.
Nature of the rash
The appearance of rashes on the body is a specific sign of meningococcal infection in children. Skin lesions occur in 70-90% of cases. Irregular rashes form on the child’s body. They can be small in diameter or merge with each other. Such manifestations are localized on the eyelids, sclera, thighs, and buttocks. With the further development of meningitis, areas with necrosis are rejected, which leads to the formation of scars. In particularly severe situations, blood poisoning may develop, which can result in death.
The main difference between a meningeal rash is that it does not rise above the surface of the dermis and has an area of necrosis in the center.
Other symptoms
In addition to the main signs of meningococcal infection in children, the following symptoms can be noted:
- necrosis of the skin. Due to the severe and prolonged course of the disease, blood vessels suffer. They develop inflammation and thrombosis. As a result, vascular ischemia and subcutaneous hemorrhages occur. This symptom is most pronounced in those areas of the dermis where there is compression. The resulting ulcers take quite a long time to heal, often accompanied by a bacterial infection, and colloidal scars are formed. Necrosis is difficult to treat;
- conjunctivitis and uveitis. Such complications are quite common with meningococcal infection. As a rule, modern antimicrobial treatment allows one to avoid severe consequences such as panophthalmitis and blindness;
- strabismus. The abducens cranial nerve runs along the base of the brain. The severe course of this type of disease is often accompanied by the development of strabismus. This occurs due to damage to this nerve and the development of paralysis of the lateral rectus ocular muscles. With proper treatment, this symptom goes away in 10-14 days;
- partial or complete deafness that cannot be treated. Such a serious complication can occur in children due to the spread of the pathogen to the area of the inner ear. Only timely treatment of meningitis helps prevent this consequence.
Based on the information described above, it is clear that the pathology has quite severe symptoms and dangerous complications in children.

When the first signs of the disease develop, you should not hesitate. Every minute that meningitis develops carries a risk of irreversible consequences.
What does the rash look like?
The rash of meningitis is called erythema because of its characteristic appearance. It appears due to the fact that meningococcal toxin paralyzes blood vessels and increases the permeability of the vascular wall. This is a hemorrhagic rash. It is an early sign of meningitis, which appears during the first hours or days of the disease.
Quite often, rashes with meningitis are difficult to notice. They are localized on the legs (buttocks, thighs, legs, feet), less often on the forearms and hands. This is due to the peculiarities of the location of skin vessels in the limbs and torso. Hemorrhagic rash with meningococcal infection rarely appears on the face.
The rash with meningitis in adults in the photo has an irregular shape. It can be red or dark brown in color, varying in size - from small dots to large bruises. The photo shows that meningitis spots rise above the surface of the skin. This is clearly noticeable to the touch.
With meningococcal infection, meningitis can be combined with meningococcemia (infection pathogens entering the blood). Almost immediately a characteristic rash appears on the child’s skin. It is initially red and then acquires a bluish tint. The rash in children first appears on the feet and then spreads to the entire body. This is an extremely dangerous symptom of meningitis. If a rash appears, the child must be immediately hospitalized and adequate antibacterial therapy must be started.
Sometimes individual elements of the rash with meningitis merge into large hemorrhagic spots. In rare cases, they can form a large area of rash in the form of gloves or socks. Spots due to meningitis in children can be seen in the photo. They are a sign of generalized meningococcal infection - sepsis. If treatment with effective antibiotics is not started immediately, the disease can be fatal.
Elements of meningitis rashes may become pigmented and then disappear. Sometimes they undergo necrosis with the formation of crusts that are rejected. In their place, shallow skin defects remain.
Expert opinion
Author:
Andrey Igorevich Volkov
Neurologist, Candidate of Medical Sciences
For many years, meningitis remains one of the most dangerous infectious pathologies. Every year, a large number of people die from this disease, which affects the meninges. Despite the treatment started, death occurs in 10% of cases. The first 1-2 days after the onset of pathological symptoms are considered the most dangerous. Meningitis ranks first among the causes of death. Doctors strongly recommend seeking help immediately. Self-medication is strictly prohibited.
Hemorrhagic rash due to meningitis is one of the main signs of the disease. Often, rashes fade into the background compared to other striking symptoms of infectious lesions of the meninges. However, it is important to take into account the entire clinical picture and not lose sight of skin changes. Neurologists at the Yusupov Hospital diagnose and treat meningitis in accordance with the latest European recommendations. Meningitis must be quickly differentiated from other infections. The coordinated work of the doctors at the Yusupov Hospital allows us to quickly and efficiently carry out the necessary research to make the correct diagnosis.
Signs of purulent meningitis
Purulent meningitis is a severe form of pathology in children, which is caused by several types of infection. The pathology is divided into meningococcal (caused by meningococcus), pneumococcal (caused by pneumococcus) and hemophilic influenzae (caused by Haemophilus influenzae).
Common symptoms in children
The onset of the disease, as with other forms of meningitis, has a rapid and acute course. From the first day of brain damage by infection, the patient’s body temperature rises to 38-39 degrees. In some cases, the child’s temperature reaches 40 degrees Celsius. It is important to note that traditional antipyretic drugs, such as Paracetamol, Ibuprofen and others, do not help normalize the temperature.
Common symptoms of purulent meningitis in children include:
- severe headache. However, it is not possible to clearly determine its localization. The pain intensifies with bright light, loud sounds, or changes in body position;
- nausea not caused by food intake. In many children, nausea is accompanied by vomiting. Antiemetic medications do not provide the expected therapeutic effect;
- photophobia. In bright light, the child experiences pain in the eyes. Unpleasant sensations intensify when trying to examine any object;
- convulsive syndrome. When trying to stretch the legs, the child experiences increased headache and tension in the back of the neck. This symptom is one of the positive meningeal signs;
- in severe cases, the patient experiences trembling of the limbs. Typically, such manifestations require immediate medical measures in the intensive care unit.
In addition, signs of intoxication of the body increase. The child’s general well-being sharply deteriorates. Children are capricious, become lethargic, and refuse to feed. Breastfed babies cry even in their arms. Due to high temperature, drowsiness and weakness develop. If left untreated, the consequences of this condition can be very negative.
Nature of the rash
What does a rash look like in children with meningitis? The appearance of a rash on the body is an unfavorable symptom during the course of the disease. This characteristic sign occurs in all parts of the body, in the oral cavity. More often it can be seen on the sides of the body, on the stomach, buttocks, and feet. The rash may have a small diameter and merge into larger formations.
What should such a rash be differentiated from?
Seeing the appearance of hemorrhagic rash elements on the child’s body, mothers may suspect a severe manifestation of an allergic reaction, for example, to a food product or a newly used cosmetic care product. The distribution frequency of such elements is quite similar.
However, with meningitis, unlike allergies, the rash: does not itch, does not hurt, is accompanied by a high temperature, does not turn pale when pressed, and is not located on the head and face in particular.

Elements of a meningeal rash appear in stages, as the next amount of meningococcus is released into the blood. Each such addition is accompanied by an obligatory temperature jump.
The distinctive features of the rash due to meningitis from other diseases of an infectious nature are:
- pale skin;
- painful sensations in joints and muscle fibers;
- peculiarities of coloring of the nasolabial fold (it becomes pale, slightly bluish);
- intermittent, somewhat labored breathing;
- increased heart rate;
- neglect of food;
- need for intensive drinking.
Manifestations of serous meningitis
It is believed that most cases of serous meningitis are caused by viral diseases. As a rule, these are enteroviruses. Less commonly, pathology is caused by mumps virus, influenza, parainfluenza and herpes. Mostly children under 7 years of age are susceptible to the disease.
You might be interested in: Pemphigus of the newborn
First symptoms of the disease
The incubation period of serous meningitis usually lasts from three to ten days. Its duration depends on the child’s immune system. After the end of the incubation period, the first characteristic signs appear:
- pain when touching the skull – Pulatov’s symptom;
- contraction of the facial muscles when trying to press on the cheekbones - ankylosing spondylitis symptom;
- the child’s legs cannot be straightened, he keeps them bent at a right angle – Kernig’s symptom;
- if you try to tilt the baby’s head forward, he will automatically pull up his legs – the upper Brudzinski’s symptom;
- involuntary pulling of the legs towards the body when pressing on the lower abdomen is the average Brudzinski symptom;
- If a child straightens one leg, the second will bend involuntarily - the lower Brudzinski symptom.
These signs can easily suspect meningitis. The symptoms can be seen in the photo.

If parents find at least one or more of them, they should definitely call an ambulance.
Clinic for further development of pathology
Symptoms indicating damage to brain tissue and nerves include:
- increased body temperature;
- decreased visual and hearing acuity;
- double vision before the eyes;
- development of strabismus;
- apathy, moodiness, drowsiness or, conversely, agitation of consciousness;
- some children experience hallucinations;
- drooping of the upper eyelid, involuntary swaying of the eyes.
Some signs may be absent or mild. This is due to the characteristics of the body of a particular child.
Nature of the rash
The appearance of a rash on the body is a rather dangerous sign, which often leads to negative consequences, the formation of ulcers. In this case, red or pink spots form on the body, which disappear for a few seconds when pressed. With the further development of the disease, these spots become darker and acquire a bluish tint with a clear center in the middle. If such a sign is detected, you should immediately call a doctor, since such rashes indicate the onset of tissue necrosis. If left untreated, the child may die.
Why a rash appears in children with meningitis: explanation with photos

Children, as a rule, are just developing their immunity, so they are at greater risk than others of developing various diseases.
The most dangerous of them is meningitis. To successfully treat a child, parents need to understand the general symptoms. Then you can promptly go to the hospital where treatment will be prescribed. One of the signs of the disease is a rash , which will be discussed in this article.
Symptoms of tuberculous meningitis
This type of disease develops when the brain is damaged by the tuberculosis bacillus. The infection is transmitted by airborne droplets and can affect children and adults. Most often, tuberculous meningitis is detected in children aged 2 to 6 years. The onset of pathology is usually acute or subacute.
First manifestations
Tuberculous meningitis in children begins with the prodromal stage. In this case, the child develops the following clinical signs:
- headache, which is more pronounced in the evening;
- repeated vomiting that is not associated with feeding;
- apathy, drowsiness;
- negative reaction to noise and bright light;
- indifference to surrounding events;
- low-grade body temperature;
- pallor of the dermis.
Parents often confuse such signs with fatigue or a cold, so they are in no hurry to consult a doctor.
Features of the further course of the disease
After a few days, the child’s symptoms worsen. The baby becomes restless, sleeps and eats poorly. The stool becomes disturbed, tachycardia and breathing problems appear. Body temperature rises to 38 degrees. After 3-5 days, the symptoms intensify again:
- meningeal signs appear – Brudzinsky’s, Kernig’s symptoms;
- convulsions and paralysis occur;
- breathing becomes uneven;
- heart rhythm is disturbed;
- strabismus and ptosis occur;
- Photophobia develops.
As with other forms of pathology, a rash may appear on the child’s body, which indicates a severe course of the disease. In the absence of medical care, death occurs in most cases.

In young infants, tuberculous meningitis is accompanied by swelling of the fontanel.
Rashes as a sign of other diseases
Doctors remind that it is not only meningitis that causes a rash to appear on the skin. You need to know how to distinguish rashes from other ailments:
- chickenpox. With this disease, the rash is more blistering and covers almost the entire body of the child. In addition, he complains of constant itching.
- measles. In this case, the rash appears on the face; with meningitis, this localization is quite rare.
- various allergic reactions. The spots have a redder tint, and the patient does not have a general infectious syndrome.
- rubella. With rubella, the spots do not merge, and the rash does not appear at the beginning of the disease, but as it progresses. In addition, with this disease a person develops a runny nose and sore throat;
- scarlet fever. This disease is provoked by streptococci, they also act as the instigators of meningitis. However, this disease does not cause itching.
- pyodemia. Here formations can spread throughout the body. It looks like bubbles.
Important! If any redness appears, regardless of the disease, you should consult a doctor.
The rash with meningitis is pronounced, but not everyone can recognize it at an early stage. Mostly, patients go to the doctor when other symptoms become apparent. The localization and nature of the rash helps to diagnose a dangerous disease in time. It must be treated exclusively in a hospital setting.
Consequences of infectious pathology
If meningitis is detected in a child in a timely manner and the necessary treatment is carried out, the consequences of its serous form, as a rule, develop extremely rarely. If there is no treatment or the disease is severe, complications may be as follows:
- decreased sleep quality;
- difficulties in perceiving information by a child;
- impaired concentration and memory;
- frequent headaches;
- convulsions, often observed at night.
The more often described consequences are mild in nature and can be observed within five years after meningitis. If a child gets sick at the age of 11-13, then until the age of 17 he may still experience various complications. In adulthood, they disappear on their own.
Complications after purulent meningitis
If in childhood the patient suffered severe purulent meningitis, the consequences may be as follows:
- speech disorder;
- decreased vision and hearing, including their complete loss;
- impaired mental development of the child;
- malfunctions of the musculoskeletal system;
- more developed epilepsy;
- paralysis, convulsions.
The purulent form of infectious pathology is considered one of the most dangerous and is difficult to treat. In this regard, the consequences of the disease can be quite serious.
Disability is one of the most severe consequences of various forms of meningitis.
Consequences of meningococcal infection
Regarding meningococcal meningitis, the following consequences can be distinguished:
- paresis, paralysis;
- hydrocephalus;
- epilepsy;
- neuroendocrine disorders;
- cerebrovascular disease;
- pyelitis, cystitis;
- exacerbation of chronic diseases.
To prevent and treat various consequences after suffering from meningitis, the patient needs competent rehabilitation, which is carried out in a hospital setting. In the future, the child is recommended to undergo sanatorium-resort treatment and attend children's health camps.
Life-threatening complications
The dire consequences of suffering from meningitis in childhood are considered to be conditions that occur in approximately 5% of patients with a purulent or complicated course of the disease. These include:
- repeated inflammation of the membranes of the brain;
- meningoencephalitis;
- disorders of the respiratory and cardiovascular systems;
- cerebral edema;
- persistent increase in intracranial pressure;
- death.
You may be interested in: Treatment of borreliosis in children
Only timely diagnosis of the disease and its competent treatment can help protect a child from the conditions described above.

Negligent attitude towards the baby’s health and attempts at self-medication, as a rule, lead to serious consequences.
Diagnostics
Meningism in children requires immediate diagnosis and treatment. In addition to checking Kernig and Brudzinski symptoms, doctors use the following methods when making a diagnosis:
- collection and examination of blood and urine tests;
- assessment of glucose, urea, creatinine and other indicators;
- swabs from the nose and mouth for pathogenic microorganisms;
- blood test for HIV infection;
- liver tests;
- study of serological blood parameters;
- biochemical analysis;
- bacterioscopy, bacteriological culture.
In addition, instrumental diagnostic methods such as computed tomography, x-ray, and electroencephalogram of the brain are used.
Often, when pathology develops, an examination by specialized specialists (neurologist, ENT specialist, cardiologist and others) is required. Only correct and comprehensive treatment will help save the patient’s life.
Laboratory indicators
It is impossible to check a child for meningitis without laboratory tests. At home, diagnosis can only be carried out by a medical professional, and the doctor takes into account the presence of positive Kernig and Brudzinsky symptoms. This test does not allow you to diagnose, but only to suspect a dangerous disease.
Further detection of the disease is carried out by assessing the patient’s biological material in the laboratory:
- A blood test helps identify the presence of meningococcal and pneumococcal infections. This is evidenced by elevated white blood cells. In this case, the leukocyte formula shifts to the left, the production of antidiuretic hormone increases, and hyponatremia develops;
- Urinalysis for meningitis shows an increase in protein concentration, often there is an admixture of blood;
- bacteriological cultures from the nose, ear, mouth often indicate the presence of meningococcal infection;
- Liver tests are performed to differentiate from other pathologies with similar symptoms.
The combination of such research methods helps confirm or refute the diagnosis of meningitis.

Without laboratory studies of the patient’s biological material and the use of instrumental diagnostic methods, it is impossible to establish a diagnosis.
Other signs of illness
A rash is considered far from the only sign of an infectious disease.
Knowledge of the clinical picture of the disease will help distinguish it from others.
The main symptoms here are:
- heat;
- headaches . They are often accompanied by nausea and vomiting, double vision and blurred vision. Sometimes there is a reaction to loud sound and bright light.
- In infants, a bulging fontanel . However, if it is overgrown, then this sign does not make itself felt.
- "cop dog" pose. This symptom is perhaps the most characteristic. In this case, the child is forced to lie on his side, with his leg bent and his back arched. This position relieves pain.
Important! A dangerous sign is a combination of fever and rash. In this case, urgent hospitalization is necessary. You cannot treat meningitis at home. This disease is very dangerous and requires constant medical supervision.
How is meningitis treated in children?
Anyone can become infected with the infection that causes meningitis. According to statistics for Russia, there are three cases of the disease per 100 thousand population. The mortality rate is about 14%. In connection with such alarming statistics, the pathology should be treated in a timely manner. Only proper therapy helps prevent dangerous consequences.
Therapy tactics
Treatment of infectious pathology is carried out in a hospital setting. In this case, complex treatment is used aimed at fighting infection, alleviating the child’s condition, preventing dehydration and other negative consequences.
Treatment tactics include the following areas:
- compliance with bed rest during the acute period of meningitis;
- dieting. Children under one year of age are advised to breastfeed. For older patients, a gentle diet using easily digestible products is recommended;
- Antibiotics are used to combat the causative agent of bacterial meningitis. Previously, pathogenic microflora is determined using laboratory tests;
- the temperature should be brought down in a timely manner with the help of antipyretic medications;
- after the end of the acute course, the child is prescribed drugs that help restore brain tissue and means to improve the metabolic processes of the central nervous system.
To prevent dangerous consequences, treatment is carried out with the help of general strengthening drugs, anticonvulsants and other medications. During the recovery period, the child needs competent nursing care, which includes measuring body temperature, assessing the general condition of the patient, monitoring blood pressure, urine output, breathing and other criteria.
Nonspecific prevention of meningitis and its consequences
To prevent meningitis and its severe consequences at any age, certain preventive measures should be followed. These include:
- timely consultation with a doctor in the event of the development of bacterial, viral and fungal diseases;
- refusal of self-treatment;
- avoiding visiting crowded places during the cold season;
- increasing immunity through proper nutrition, sports and frequent walks in the fresh air;
- compliance with personal hygiene rules;
- timely treatment of dental diseases.
It is especially important to follow these recommendations among patients at risk (children under 7 years of age, patients with cerebral palsy, patients with reduced immunity, and other birth defects).

Following simple preventive rules will help to significantly reduce the risk of infection and the development of severe consequences.
Do I need to get vaccinated?
On many forums you can find active discussions and reviews about vaccinating children against meningitis. Some argue that this is the only way to protect their child from pathology, while others are categorically against it. Experts' opinions on this matter are also divided.
Due to the fact that meningitis is caused by various bacteria and viruses, there is no single vaccination that could protect against all these diseases. To prevent dangerous consequences in medical practice, a vaccine is used that helps develop immunity to the most dangerous among them (Haemophilus influenzae, pneumococci, meningococci).
Types of vaccines and their names
In the table you can find the names of the vaccines that are most often used to protect against meningitis.
| A drug | From what age is it used? | Manufacturer | Price in rubles |
| Menactra | 2 times before the age of 2 years After 2 years once | America | 4100 |
| Mencevax | After 2 years | Belgium | 1471 |
| Meningococcal | 1.5 years | Russia | 742 |
| Meningo A+C | After 2 years | France | 4900 |
The prices for vaccines are approximate; the exact cost should be checked with the seller.
Main classification of meningitis
The bacteria that cause the disease are very common: almost one in ten of us have the same bacteria that cause meningitis in our nasopharynx, and for most of us it is harmless. Bacteria are spread from one person to another through close contact (eg coughing, sneezing, kissing). The bacteria cannot live for more than a few moments outside the human body, so they are not transferred to things such as clothing and bedding, toys or food.
How does the disease occur, why can some children develop meningitis or sepsis? Scientists don't yet fully understand why some people get sick from germs that are harmless to most of us. However, it is known that infants and young children are at greater risk than older children and adults, in part because their immune systems are not yet fully developed.
The disease is conventionally divided into the following forms:
- Purulent;
- Serous.
Purulent meningitis
Purulent meningitis in children is caused by meningococci, Haemophilus influenzae, and pneumococci. We are talking specifically about a bacteriological infection, which causes an “attack” of leukocytes. Mostly this type of meningitis affects children under 1 year of age. An extremely dangerous form of the disease! Without treatment, this form of meningitis leads to death in 50% of cases. Even with early detection of the disease and timely treatment, mortality is up to 10% within 2 days (usually within 24 hours) after the first signs of the disease appear.
Serous meningitis
Serous meningitis in children can be caused by both viruses and fungi. Most often, this form of the disease begins with a sharp increase in body temperature up to 40 degrees. And it is extremely difficult to accurately determine that it is meningitis, since upon visual examination of a child, the disease can easily be confused with the ordinary form of influenza. Suspicion can only be caused by excessive tension in the neck muscles and the child’s constant complaints of headaches.
The meningococcal vaccine provides very good protection, but does not protect against other forms of meningitis and sepsis caused by other bacteria, so it is very important to know the symptoms and signs of meningitis in children of different ages.










