Pneumonia in children - symptoms:
- Headache
- Weakness
- Nausea
- Fever
- Dizziness
- Abdominal pain
- Vomit
- Chills
- Sweating
- Drowsiness
- Cough
- Chest pain
- Labored breathing
- Hard breath
- Rapid breathing
- Flatulence
- Refusal to eat
- Coughing up blood
- Blue discoloration of the nasolabial triangle
- Moodiness
- Sputum in the form of rust
What is pneumonia in children
Pneumonia in children is a serious inflammatory disease that affects the respiratory sections of a child’s lungs. The pathology can have a different etiology, but is always severe, and children under 3 years of age suffer from pneumonia three times more often than older children (from 3 to 16 years).
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
Predisposing factors for newborns are perinatal pathologies, congenital heart and lung defects, immunodeficiency states and hypovitaminosis, as well as rickets - in such cases congenital pneumonia develops.
Predisposing factors for older children may include:
- passive smoking;
- the presence of foci of chronic infection and other pathological conditions in the body.
At the same time, you need to understand that for the onset of the disease a necessary condition is the presence of such a predisposing factor as hypothermia of the child.
Symptoms of pneumonia in patients aged 1-3 years
What signs are characteristic of bilateral pneumonia in children (see photo below)?

These include:
- high temperature lasting more than three days;
- hard breathing, which can be heard with a phonendoscope;
- retraction of the intercostal spaces during inspiration;
- shortness of breath, that is, the presence of more than 40 respiratory acts within a minute;
- bluish skin;
- symptoms of intoxication in the form of weakness, lethargy and drowsiness.
Causes of pneumonia in children
There are a lot of bacteria and viruses that can cause the development of this disease in a weakened child’s body. In particular, pneumococci are the most common pathogens, but there are other bacteria that can cause this disease, and these are:
- chlamydia;
- staphylococci;
- Pseudomonas aeruginosa;
- streptococci;
- Proteus;
- E. coli, etc.
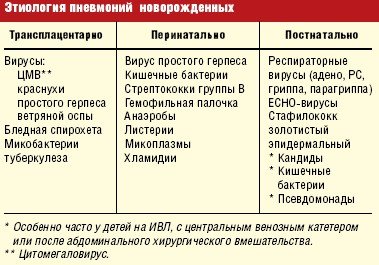
Etiology of pneumonia in newborns.
The pathogen enters the body through the respiratory tract, enters the lung tissue and infects the alveoli. Depending on the type of pathogen, there are several forms of pneumonia in newborns:
- bacterial and fungal;
- mycoplasma and viral;
- rickettsial;
- a disease resulting from helminth infestation.
In addition, pneumonia in children can be allergic in nature and be associated with the fact that the baby’s body is not yet fully formed and cannot adequately respond to certain irritants. Pneumonia in newborns can also be caused by exposure to a variety of chemical or physical irritants.

Separately, it is necessary to say about pneumonia in newborns and older children caused by viruses. They are also divided into several groups, depending on the type of virus, and are:
- influenza;
- parainfluenza;
- adenoviral;
- respiratory syncytial.
As mentioned above, for the development of pneumonia in a child, predisposing factors must be present. The following states can be added to those listed earlier:
- prematurity;
- hypovitaminosis;
- cystic fibrosis;
- intrauterine hypoxia;
- birth injuries.
And all children are given vaccinations at birth, which are designed to protect the child from various pathologies. And such a vaccination can cause a decrease in the protective reaction of the baby’s body, as a result of which pneumonia can develop.
Pathogens and risk factors
Children are at risk for the following reasons:
- Due to the age-related characteristics of the structure of the trachea and large bronchi: in children their length is much less, and they themselves are wider than in adults, which facilitates access to the lungs of pneumonia pathogens, and the structure of small bronchi and vesicles, on the contrary, is thinner, more delicate with a narrow lumen, so they tend to become obstructed faster. Also in children, the bronchial system is poorly differentiated, which makes natural drainage difficult and creates a favorable environment for inflammation.
- Features of the structure of lung tissue in children: increased likelihood of developing emphysema and atelectasis due to a lack of surfactant and elastic fibers.
- Physiological features of the children's bronchopulmonary system: weak activity of the processes of removing small foreign particles and mucus, weak immunological activity due to underproduction of interferon and immunoglobulin A.
- The presence of a number of diseases that weaken the immune system: anemia, blood diseases, diathesis, rickets, heart and lung defects, metabolic disorders, etc.
- The presence of diseases that directly provoke pneumonia, such as acute bronchitis, bronchiolitis and bronchopneumonia.
- In newborns and children under 2 years of age: the presence of infections during pregnancy in the mother, low birth weight, artificial feeding.
- Environmental factors: long stay in the hospital, contact with patients with pneumonia.
Pneumonia is polyetiological. It is characterized by a wide range of pathogens; it is more convenient to present them by types of pneumonia in children:
- “domestic” or community-acquired pneumonia is caused by pneumococci, viruses, Haemophilus influenzae and intracellular pathogens;
- Pneumonia in newborns is caused by viruses and intracellular pathogens;
- aspiration pneumonia is caused by gram-negative flora and obligate anaerobic bacterial organisms;
- hospital-acquired pneumonia is caused by staphylococci and gram-negative flora;
- immunodeficiencies are accompanied by the invasion of various pathogens.
According to statistics, in newborns and children under 1 year of age, the most common pathogens are Haemophilus influenzae and pneumococci, but chlamydia, E. coli pathogens, staphylococci and pneumocystis are also found. Pneumonia in children of other ages is characterized by damage to mycoplasmas, pneumococci and chlamydia.

Classification of the disease
In modern medical practice, pneumonia in newborns is classified not only by etiological signs, but also by causal ones. Taking into account the cause of pneumonia in a child, pneumonia is divided into primary and secondary. Primary occurs when an infection enters the baby’s body, and secondary occurs as a consequence of other foci of infection existing in the child’s body.
In addition, the disease can be classified according to the nature of its course. It could be:
- acute pneumonia in children;
- subacute form of the disease;
- protracted.
According to the degree of damage to the lung tissue, several types are distinguished - the disease can affect one lung or two at once (one or two-sided pneumonia) and most often it is the right one that is affected - right-sided pneumonia develops.

What kind of disease is this?
Damage to the lungs to the same extent is very rare. The picture of pathology in these respiratory organs sometimes has significant differences. For example, in one lung there may be focal inflammation, while in the other several segments are simultaneously affected.
The causes of double pneumonia in a child can be infections:
- bacterial;
- viral;
- fungal.
But most often, inflammatory processes in the lung tissues occur due to pneumococcus. These microorganisms affect the respiratory system, which provokes the development of gas exchange disturbances, the rapid progression of intoxication, as well as oxygen starvation.
Symptoms of pneumonia in children
Depending on the type of disease, signs of pneumonia in children can be very diverse. Nevertheless, there are some symptoms characteristic of each type of pneumonia, these are symptoms of general intoxication:
- heat;
- drowsiness and weakness;
- refusal to eat;
- cyanosis of the nasolabial triangle;
- unreasonable sweating;
- rapid, heavy breathing;
- headache (moody in young children due to pain symptoms).
To distinguish the signs of pneumonia in a child, you need to know how this or that type of pneumonia manifests itself:
- focal pneumonia in children. A disease that affects only a small area of the lung. It is the mildest form of the disease and can sometimes occur hidden, without any particular symptoms or with unexpressed symptoms. The source of infection can be located in any part of the lung - often in young children, hilar pneumonia occurs, which is characterized by damage to the root of one or two lungs, and is characterized by severe intoxication and severe symptoms;
- segmental pneumonia in children. We talk about this disease when individual segments of the lung are affected. The disease begins abruptly and is characterized by an increase in temperature to high numbers and a rapid increase in symptoms of intoxication. A newborn's cough with pneumonia is absent or mild, while the baby feels pain in the chest or abdomen and difficulty breathing. Diagnosis of this disease is carried out on the basis of radiography methods - the x-ray shows individual affected lobes merging into a single segment;
- lobar pneumonia in children. A disease in which the process involves not only a lobe of the lung, but also part of the pleura. As with segmental, the onset of the disease is acute. The temperature rises, the child complains of dizziness and nausea, and chills are observed. Newborn babies often cry, breathe heavily and their temperature also rises, which can reach critical values. Cough with this type of pneumonia in newborns is rare, and in the first 3 days it may even be completely absent, then it becomes dry, and after a few days rust-like sputum appears. Often the course of the disease is associated with the appearance of abdominal syndrome (especially in young children), which is manifested by flatulence and vomiting. Only an experienced doctor can diagnose the disease - based on X-ray data, anamnesis and physical examination of a small patient. A blood test taken from a child with lobar pneumonia will show a shift in the leukocyte count to the left, an acceleration of the ESR;
- interstitial pneumonia in children. This type of disease is less common than others - it often occurs in premature babies, as well as in newborns with immunodeficiency conditions. In addition to the symptoms described above (hyperthermia, excessive sweating, etc.), interstitial pneumonia of newborns is characterized by changes in the gastrointestinal tract, a drop in blood pressure and disturbances in the functioning of the nervous system. This type of pneumonia is characterized by a debilitating cough with scanty sputum, and you can also visually observe swelling of the chest.
Focal pneumonia in children
General picture of the disease manifestation
Bilateral pneumonia in a child under one year of age is characterized by extensive damage to the lung tissue. Moreover, the more active and larger the foci of pathology, the more severe its course will be. In addition, the course of the disease in children under one year of age is characterized by good reactivity to the influence of antibacterial agents. If the course of therapy is started on time and correctly prescribed, the problem can be eliminated within one week.
Pneumonia in children begins in the form of a cold. Symptoms such as cough and runny nose gradually develop. The respiratory tract is affected by a bacterial infection, which, as the pathology progresses, penetrates into the body. It is believed that at the initial stage it is very difficult to diagnose pneumonia in young children. After all, babies are not able to cough effectively, that is, show the main symptom of pneumonia. In addition, the doctor cannot always listen to wheezing in infants. In this regard, suspicion of the disease arises only when a combination of such signs as:
- rapid breathing;
- shortness of breath;
- blue discoloration that appears in the area of the nasolabial triangle;
- loss of appetite;
- temperature increase;
- drowsiness.
Severe cases of the disease in infants under one year of age are accompanied by convulsions and pulmonary failure, as well as very severe shortness of breath. When a sick child inhales, the wings of the nose widen, and the noise from breathing can be heard even at a distance from him.
Pneumonia is diagnosed at such an early age only on the basis of data obtained as a result of radiography. This study allows us to clarify the type of illness. Treatment should be started immediately.
Diagnostics
As mentioned above, one or another type of pneumonia is diagnosed in infants and older children on the basis of bacteriological tests, radiography and local examination. In particular, they check the temperature reaction, the presence of signs of respiratory failure (shortness of breath, cyanosis of the mucous membranes and skin).
Patients are prescribed a blood test, which notes leukocytosis, increased ESR and neutrophilia. X-rays confirm the damage to a certain lobe, segment or the entire lung.
It should be noted that the most severe prognosis for the course of the disease is in newborns, since their body is weak and cannot cope with the infection on its own. Moreover, such children often experience destruction of lung tissue, which can lead to death. Therefore, the earlier pneumonia is detected in a small child and the sooner its treatment is started, the better the prognosis.
Stages of pneumonia
Light form
The main symptom is an increase in body temperature to 39 °C. General health is slightly affected. The breathing rate periodically increases. Blood gases are normal.
Moderate form
Symptoms of intoxication begin to increase, and appetite decreases. The child becomes lethargic or, on the contrary, restless. When screaming, cyanosis increases. Shortness of breath increases.

Rice. 10. Photo of a sick child.
Severe (complicated) form
Shortness of breath and palpitations increase. The balance of acids and alkalis (acid-base balance) is disturbed in the child’s body. All symptoms of intoxication worsen. Infectious-toxic shock may develop. Body temperature rises to 40 °C and above. Severe acrocyanosis. One of the serious complications is the collapse (destruction) of lung tissue.
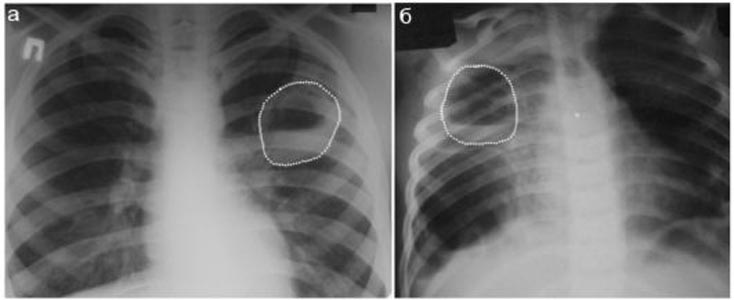
Rice. 11. A drained lung abscess in children (dotted line) looks like a delimited cavity with a fluid level.
Treatment of pneumonia in children
Newborns suspected of having this disease are subject to immediate hospitalization. The hospital also provides treatment for pneumonia in children with moderate and severe forms of the pathology. Children aged 3 years and older in the presence of the initial stage of the disease with mild symptoms can be treated at home, with the necessary medical supervision several times a week. It should be remembered that the consequences of pneumonia can be the most severe - often, if not treated in a timely manner, children experience damage to internal organs and the central nervous system.
Treatment of the disease should be comprehensive and include:
- drug therapy;
- physiotherapy;
- normalization of diet and drinking regime.
The main place in the treatment of pneumonia is given to antibiotics. Within a day after the start of treatment, the condition improves, provided that the drug is selected correctly, taking into account the sensitivity of the pathogen to it. The treatment process takes from 6 to 10 days, depending on the severity of the little patient’s condition.
If the disease is caused by viruses, antiviral drugs are prescribed. Immunostimulants and mucolytics are also indicated. Antipyretic drugs are prescribed if the child’s temperature rises above 38.5.
Depending on the symptoms, other medications may also be prescribed to maintain and protect other organs and systems. For example, antihistamines, corticosteroids, cardiac glycosides. Breathing exercises are mandatory, helping the child’s lungs restore their functions (for children over 3 years old) and massage, which is suitable for children of any age. Sometimes it is necessary to take medications that reduce bronchospasm - in this case, the child is prescribed aminophylline.
The prognosis for treating the disease is favorable, provided that treatment is started in the early stages of the disease. The child is discharged from the hospital after completing the course of antibiotics, but at home he still needs symptomatic treatment to eliminate residual effects.
In addition, prevention of pneumonia in children plays an important role in preventing relapses of the disease. Doctors recommend using traditional medicine in the post-clinical period to eliminate the consequences of the disease and increase immunity. In particular, inhalations with fir oil, consumption of radish with honey, cabbage juice with honey as an expectorant, a mixture of butter with propolis as an immune-strengthening agent, etc., help well.
Pneumonia in children treatment methods
If signs of pneumonia appear, you should contact your pediatrician.
The famous children's doctor Komarovsky identifies several specific symptoms that are the basis for a visit to a specialist:
- cough is the main sign of pathology;
- the child’s condition worsened after improvement;
- manifestations of a viral infection are observed for more than a week;
- when breathing deeply, coughing attacks occur;
- there is severe pallor of the skin;
- shortness of breath occurs;
- the use of antipyretic drugs does not produce results.
The choice of treatment method depends on the causes and severity of the disease. It is very important to start treatment as early as possible - this will make it as effective as possible.
How can you identify pneumonia in a child?
Every parent sooner or later asks the question: how to determine pneumonia in a child? This disease manifests itself in children more often than other diseases. Intensive development of medicine over the past 50 years has been able to mitigate the impact and consequences of the disease.

The child’s recovery occurs in almost all cases (provided parents contact doctors in a timely manner). Pneumonia in most cases is caused by infectious causes. The most common factor is considered to be bactericidal viruses (pneumococci), which find a permanent home in the nasal cavities.
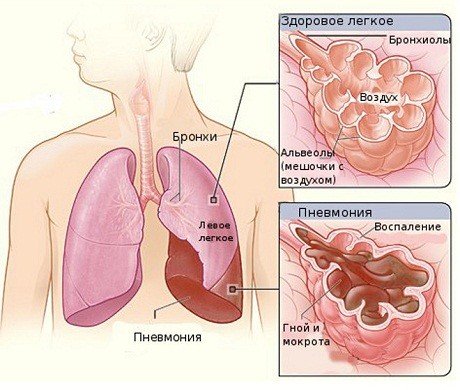
At the age of six, the disease is provoked by Haemophilus influenzae. A school-age child is exposed to chlamydia, mycoplasma, which is a viral source of such pathology. One of the key tasks of the lungs is to supply oxygen to the body. The communication of oxygen in the body occurs due to vascular channels that perform the transport task. The important task is carried out by the alveoli (small sac-like areas of the lung). Under normal operating conditions, the alveoli do not disintegrate together when air is exhaled.
Pneumonia strikes precisely in these areas, filling them with products of the inflammatory process. The result of this process is a malfunction of the entire lung, as a result of which harm is caused to the body through inflammatory fluids.
Children were the first to experience the success of medical developments in the fight against pneumonia. Relatively recently, this disease was considered a serious enemy to the health and even life of the patient. Today, pneumonia as a fatal disease is no longer scary. However, a positive treatment result depends on high-quality, quick diagnosis and, accordingly, well-designed therapy.
Factors that provoke pneumonia in children
The group of factors causing the disease is headed by bactericidal viruses. The ARVI viral group cannot be excluded (both the cause of pneumonia and a means of transporting other viruses to the lung area). Some cases of the disease can be caused by fungal viruses or intracellular microbes.
Intrauterine pneumonia is no exception. Viral trace elements affect amniotic fluid due to the placenta at the time of fruiting or the birth canal, which is subject to an inflammatory process. As a result, a newly born baby may already be sick with pneumonia.
Parents should be aware of how pneumonia can be recognized in order to detect the disease in a timely manner.
Children at risk
The following factors are characteristic of the group of children most predisposed to this disease:
- the weight of the born child is quite small;
- during pregnancy, the mother suffered a viral or bacterial disease;
- iron deficiency anemia;
- heart defect;
- rickets;
- affected nervous system;
- long period of stay in a stationary unit.
In the latter case, the likelihood of pneumonia is very high. The causative agent of the disease in this situation is an aggressive flora with a negative reaction to antibiotic drugs.
Symptoms of pathology
An experienced practitioner is able to establish the correct diagnosis of the disease and determine a successful course of treatment. In some cases, diagnosis of pneumonia requires X-ray results. Do not be afraid to use such an analysis method, since the quality of determining the disease will only increase, which may well compensate for the negative impact of X-rays on the baby’s body.
A person with pneumonia experiences the following symptoms:
- a bluish color of the skin and lips appears;
- lack of appetite;
- retraction of the soft tissues of the baby’s chest;
- feeling of anxiety, increased drowsiness;
- increased breathing (age up to 2.5 months - 60 times per minute, 2.5 months - 1 year - more than 55 times, 1-3 years - more than 40 times);
- the respiratory tract wheezes;
- temperature above 38º C for 2-3 days.
An extensive inflammatory process is expressed by shortness of breath, in which the soft spaces between the ribs can be drawn inward.
The respiratory process involves the nasal and cervical muscle groups. Children have a natural desire to sit down or raise their arms and shoulders higher. This desire is explained by the fact that in this position the chest expands and breathing becomes a little easier. At the same time, a pale blue tint appears on the lips and the edges of the nose. If these symptoms occur, you should immediately seek hospital treatment, because the risk of death increases due to disruptions in the central nervous system due to oxygen deficiency.
Diagnostics of newborns
It is necessary to pay attention to the baby's behavioral changes. Lethargy appears, in rare cases - anxiety, moodiness, loss of appetite. Disruptions occur in the respiratory processes: rhythm is lost, breathing is predominantly shallow, which involves additional muscle groups. Body temperatures rise, but in rare cases quite high. The presence of a cough is uncharacteristic. Diarrhea may occur.
One-year-old and six-year-old children with pneumonia change in behavior, shortness of breath, high fever, loss of appetite, and do not want to drink. A pale blue tint to the nose and lips occurs at the last stage of the pathology. The presence of cough is not always observed. Due to oxygen deficiency, there is a high probability of diarrhea.
Using a phonendoscope, even a qualified doctor is not always able to determine the presence of pathology. This is the insidiousness of the disease. Any diagnosis of pneumonia is based on x-rays of the lung.
Method of treating the disease
The negative impact of pneumonia affects cardiac activity and a number of important organs. A serious complication may be the appearance of purulent cavities in the lungs.
A severe form of the disease requires hospital treatment, but many patients with mild pathology cope with the disease at home. Often, a doctor cannot diagnose pneumonia during a house call. In such cases, the child and his parents are sent to the children's clinic. With effective inpatient treatment of the baby, the process can be completed at home (subject to the necessary requirements for maintaining the patient). The advantage of treatment at home lies in the atmosphere that is native to the child, eliminating the possibility of contracting the virus again in the hospital. There are many viral microorganisms in the hospital that have developed a certain immunity to antibacterial drugs.
It is the use of antibacterial drugs that is aimed at combating pneumonia. A mild form of the disease is treated with prescribed penicillin drugs administered orally. The accompanying medication is a macrolide. The second line of medications does not need to be prescribed during the initial stages of therapy. A complex form of the disease requires the prescription of injectable antibiotic drugs. After using several injections, the doctor observes the patient’s condition. If you feel better and the temperature drops to less than 38.2º C without using fever relievers, the intramuscular administration of antibiotics is stopped, and oral medication is prescribed.
When the baby's temperature has returned to normal, the patient is recommended to sleep in the fresh air (within reasonable temperature limits). Older children can go outside three weeks after the disease, but only if the treatment results are effective and in the absence of key signs of pathology. If the treatment was completed without any complications, specific rehabilitation exercises are not prescribed.
respiratoria.ru>