Streptoderma - what is it?
Streptoderma is the name given to extensive lesions of the skin of a purulent-inflammatory nature. First, spots of various sizes appear on the skin, then wounds that do not heal for a long time.
Various forms of skin pathology are caused by exposure to streptococci.
These representatives of opportunistic microflora live in the body of almost every person - in the respiratory organs, on the skin, in the gastrointestinal tract, on the mucous membranes.
Typically, bacteria from the Streptococcal family do not pose a danger; their “behavior” is controlled by the immune system. But under certain conditions, microorganisms become active and provoke various diseases.
The causative agent of streptoderma is one of group A streptococci - hemolytic.
It can also cause the development of:
- bronchitis;
- tonsillitis;
- scarlet fever;
- meningitis;
- pneumonia;
- osteomyelitis;
- erysipelas;
- sepsis;
- endocarditis.
L01 - streptoderma has this code according to ICD-10 (International Classification of Diseases). The disease occurs in the presence of a pathogen - streptococcus and damaged skin.
When the skin is healthy, the pathogen does not cause harm. But any damage allows bacteria to actively multiply and provoke inflammatory processes.
Danger comes from abrasions, scratches, cuts, scratching due to allergies and insect bites, other skin damage, even outwardly invisible microtraumas.
Ointment for streptoderma in children
Friends, here are the names of ointments that can be used in the treatment of streptococcus.
- Zinc or salicylic acid - they soften affected areas with sores, dry out and relieve inflammation. Do not use for purulent complications
- Baneocin. An excellent powder that contains an antibiotic.
- At home, streptoderma can be treated with Levomykol, Tyrose gel, and Syntomycin ointment. This treatment of streptoderma is carried out in children on the face, head, buttocks, buttocks and other parts of the child’s body.
Causes
Why are children especially susceptible to streptoderma? The fact is that they have not yet developed sufficient protective functions of the skin.
And the kids are not yet accustomed to the rules of basic hygiene. As a result, streptoderma is the most common dermatological problem among them.
The main causes of the development of skin diseases are:
- decreased body immunity;
- violation of skin hygiene rules;
- contact with a patient with streptoderma, use of shared hygiene items and utensils;
- stressful conditions, overwork;
- hormonal imbalance;
- changes in the acid-base balance of the skin (pH) – streptococcus is most active if an alkaline environment predominates;
- chronic diseases;
- climatic factors - frostbite, sunburn, temperature changes.
Streptoderma can be primary - when the pathogen enters the body through damaged skin, and secondary - streptococcal infection joins another disease that is already progressing (herpes, eczema, chickenpox).
About the causes of occurrence, routes of transmission, incubation period and places of localization of streptoderma in the following video:
Causes, risk factors
Bacteria often enter the epidermis through external skin lesions . This can be caused by various injuries: scratching, cuts, abrasions.
Streptococci also enter the body when allergic reactions occur in it: general weakness of the body and blisters on the skin are the best “atmosphere” for infection with infectious viruses.
What causes streptoderma in children? Prerequisites for development:
- general decrease in immunity;
- overwork;
- stress, nervous shock;
- poor personal hygiene;
- predisposition of the skin to damage.
When streptoderma occurs, it is necessary to treat not only it, but also the factors that caused it, in order to exclude relapse of the disease.
Streptoderma is a streptococcal skin infection, video from the “Live Healthy!” program:
Contagious or not and how it is transmitted to others
There are not so many ways of transmitting streptoderma:
- Contact – direct close communication with the sick person through hugs and kisses, joint games.
- Contact-household - infection occurs through the use of shared utensils, clothes, toys, and linen with the patient.
- Airborne is an extremely rare route of infection, when the pathogen enters the skin when a sick person coughs or sneezes.
In the case when streptoderma occurs as a result of infection from a patient, the disease develops more actively and aggressively, is more severe and lasts longer.
The disease often takes the form of an epidemic - when the sick person infects the rest of the children in the group, class, hobby group or sports section.
The duration of the incubation period varies - from 2 to 10 days, depending on the state of the immune system.
Infection with streptoderma is possible only from a sick person. Animals are also susceptible to this disease (especially cats), but they can only infect their fellow animals.
Folk remedies for streptoderma
How it begins, causes, types, symptoms, photos and treatment with drugs, all this is behind us, now the time has come for traditional medicine.
- For a one-year-old child, treatment can begin with healing of ulcers and wounds. A walnut will help with this; you need to take the leaves of the tree or the partitions from the fruit, pour boiling water over it and let it stand for a couple of hours. This infusion should be applied as a lotion for 15 minutes several times a day.
- At home, I recommend treating streptoderma in children with a decoction of oak bark. You can get the crushed bark yourself, or you can buy it at the pharmacy. Make a steep decoction and boil it for about 30 minutes. Wipe the affected areas on the face, legs and arms with the cooled medicine up to 4 times a day.
- A decoction of string and sage will also relieve the symptoms of this disease.
Treatment of streptoderma in children - Komarovsky
How quickly you can cure streptoderma in a child depends only on you. Once again, I recommend that you familiarize yourself with the photo, carefully consider what streptoderma looks like on the legs, face and arms, consolidate the information on how streptococcus begins in children, how to treat it in a child, what is treatment at home, how is it transmitted, is it contagious and what ointments can be used.
Take care of your children. Nina Kuzmenko was with you. Share information, click on social media buttons.
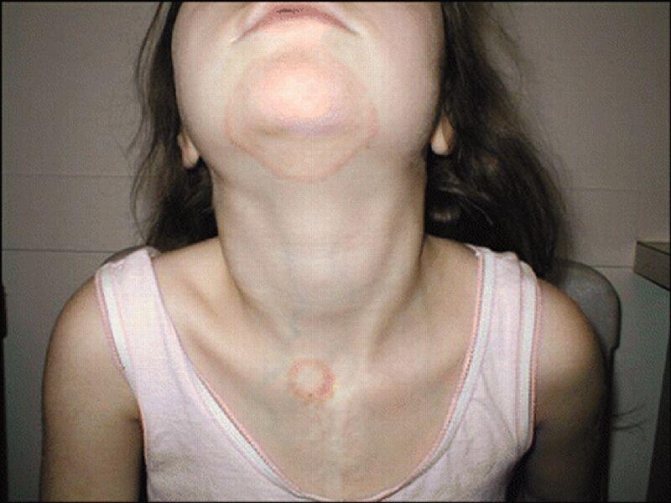
Photo: what the disease looks like when it starts
Streptococcal (contagious) impetigo

Bullous impetigo

Slit impetigo

Streptococcal diaper rash

Tourniol

Streptococcal ecthyma vulgaris

Erythematosquamous (dry) streptoderma

Papulo-erosive streptoderma
Dry streptoderma in children in the photo
This is what dry streptoderma looks like in children, which occurs without blisters and vesicles. Spots appear on the child’s body, which begin to become covered with scales in several layers; with such symptoms of streptoderma, there is no itching. This type of infection is much easier to tolerate, and most often parents confuse the symptoms with an allergic disease.

Dry streptoderma also requires treatment. The most commonly used are ointments and lotions.
Symptoms and signs
How to determine that a patient has streptoderma and not some other skin disease?
Typically, signs of the disease appear a week after infection, when the incubation period ends. At the initial stage of the disease, symptoms can be general and specific.
Of the common symptoms inherent in many infections, it is worth noting the appearance in the patient:
- high temperature - from 38°C and above;
- pain in joints and muscles;
- nausea and vomiting;
- inflamed lymph nodes.
Both adults and children infected with streptoderma experience a general deterioration in their health. This manifests itself in the form of weakness, lethargy, sleep disturbances and lack of appetite.
Characteristic signs characteristic of this particular disease help to diagnose streptoderma:
- the skin turns red and peels in different places;
- then so-called conflicts appear in these areas - bubbles with transparent liquid contents;
- these formations actively grow, sometimes reaching 3 cm, conflicts can even form a continuous surface on some part of the body;
- mature blisters begin to burst, and ulcers with jagged edges form in their place;
- these erosions dry out within a day, becoming covered with crusts that will soon fall off.
All this time, the patient experiences severe itching in the affected areas. But under no circumstances should you scratch the sores, otherwise the infection will spread throughout the body.
Each type of streptoderma has its own characteristics. For example, superficial panaritium affects the skin around the nail plate, and with slit-like impetigo, “jams” form in the corners of the mouth. We wrote about the causes and treatment of sticking in the corners of the lips here.
How long does streptoderma last? If you follow all the doctor’s instructions, you can cope with the disease within a week. In the absence of proper treatment, the process will drag on for a long time.
The video will tell you about the symptoms and signs of streptoderma:
Childhood illnesses with skin rashes
Many childhood diseases are accompanied by different types of rashes - blisters, pimples, acne, multi-colored spots, types of rashes can be seen in the photo. Skin manifestations are inherent in infectious and non-infectious pathologies.
Infectious diseases
Infectious diseases develop when pathogenic viruses, bacteria, fungi and parasites enter the body.
Types of viral rashes
Skin rashes are one of the main signs of infectious viral childhood pathologies; for each disease, the nature of the rash, its location and time of appearance are different, which greatly simplifies the diagnosis. Diseases are transmitted by airborne droplets, nutrition, and contact.
Diseases in which viral exanthems appear:
- Measles is caused by an RNA virus. A papular rash, light spots on the bridge of the nose and behind the ears become noticeable 3-4 days after infection. Gradually, the rash spreads to the face, chest and upper back, skin of the arms and legs. Additional symptoms are cough, runny nose, conjunctivitis.
- Rubella is caused by togavirus. A rash in the form of small pale pink spots appears already on the first day of illness, first on the face, then moves to the sides of the torso, buttocks, arms and skin of the legs. Additional symptoms are joint pain, sleep disturbance, weakness, temperature rises to 39.5 degrees or more. The disease is most often diagnosed in children aged 6 months to 2–4 years.
- Chickenpox is caused by the herpes virus type 3.4, the disease is most often diagnosed in preschool children and primary schoolchildren. Vesicles cover the face, body, and sometimes mucous membranes, but there are no vesicles on the feet and palms. The first rashes appear on the face, scalp, groin and genital area, the child is bothered by severe itching, and in children the temperature rises briefly to 38–38.5 degrees.
- Infantile roseola is caused by herpes virus type 6.7. The child’s temperature rises sharply, but there are no other manifestations of disease; after 4–5 days the levels also drop sharply, and a rash appears on the body.
- Warts and papillomas are small pink or brown growths that can be flat or raised above the surface of the skin. Infection with papillomavirus occurs through close contact with a sick person, but pathology develops only when cellular immunity decreases.
- Herpes simplex is a viral infection in which blisters form on the mucous membrane and skin of the mouth, nose, and around the lips.
- Infectious mononucleosis is caused by Coxsackie enterovirus and Epstein-Barr virus. Generalized infection is accompanied by pain in the liver and spleen, swelling of the tonsils. Rashes in the form of red spots 5–15 mm in size appear on days 5–7 of illness, gradually merge, and are most often localized on the face. A special feature is that with mononucleosis the rash does not itch.
- Erythema infectiosum is caused by parvovirus. At the initial stage of development, the disease occurs like a cold; after a few days, numerous red pimples appear on the face and body.
- Molluscum is a viral infection; children most often become infected in swimming pools or when using hygiene items from a sick person. Initially, neoplasms appear under the skin; as the disease progresses, they come to the surface in the form of nodules; after opening, a white heterogeneous mass can be seen inside; it contains many viruses.
Bacterial diseases
In children, bacterial diseases with skin manifestations most often occur against the background of infection with streptococci, staphylococci; microbes enter the body by airborne droplets, through wounds and scratches on the skin.
READ ALSO: How to remove blackheads in the ears and whether you can do it yourself

Scarlet fever first appears on the face and then moves to other parts of the body
Types of pathologies:
- Scarlet fever is caused by streptococci from group A. The rash can appear within 24 hours after infection - extensive red roseola with small pink dots inside appear on the cheeks, rough to the touch, they gradually turn pale and turn brown. The rashes from the face spread to the stomach, back, neck, and thighs, but there is no rash in the area of the nasolabial triangle. Additional symptoms are fever, sore throat, diarrhea, the tongue is covered with a white coating, but after a day it turns red, and papillae are clearly visible on the surface.
- Erythema migrans is a bacterial dermatosis that occurs after a tick bite. After 1–2 days, a round spot appears at the site of the bite, the skin inside turns red, peels, and the inflammation gradually grows. Itching, tingling and irritation occur only if the bite occurs in an area with thin, sensitive skin. Without proper treatment, the infection spreads to the central nervous system and meningitis may develop.
- Folliculitis, furunculosis, carbunculosis - inflammation of one or more hair follicles, often the pathological process spreads to surrounding tissues. The affected areas are red and hot to the touch, and the disease is often accompanied by fever.
- Hidradenitis - ulcers form in the sweat glands, the rash is localized in the armpits, in the groin area, in the folds of the skin, the disease develops only in adolescents.
- Streptoderma - on the face and limbs, in the folds of the skin, bubbles with purulent contents appear, which easily burst, blisters and red ulcers form.
- Ecthyma - the skin becomes covered with deep ulcers with a diameter of 2–4 cm, the inflamed areas have a soft bottom and are covered with dry crusts.

Ecthyma is accompanied by skin ulcers
Newborns are sometimes diagnosed with sexually transmitted diseases - syphilis, genital herpes, chlamydia; infection occurs in utero or as the child passes through the birth canal. Venereal rashes are varied - maculopapular rash, erosions, ulcers, chancre, nodules, they appear on the genitals, in the folds of the skin, on the face, and less often they can be found on the mucous membranes. STDs are often detected in adolescents who begin sexual activity early and have poor understanding of safe sex issues.
Parasitic infections
Parasitic diseases occur when infected with lice and mites; the pathologies are very contagious and spread rapidly in children's groups.

Pediculosis manifests itself as severe itching of the head and spots on the skin
List of common diseases:
- Pediculosis is an infestation of lice. The disease is accompanied by severe itching, red dots appear on the skin, and there are many nits on the hair.
- Scabies is an infection with the scabies mite. Scabies are formed on the skin - small winding lines of pink or gray color; the disease is characterized by severe itching, which intensifies at night.
- Demodicosis is an infection with the demodex mite. The disease manifests itself in the form of rosacea and granulomas; sores on the face are accompanied by severe itching of the eyes and profuse lacrimation.
Fungal pathologies
Mycoses occur with the active growth of pathogenic fungi; they often affect not only the skin, but also the hair and nail plates; rashes usually affect large areas. The causes of diseases are long-term use of antibiotics or the use of antiseptics, disruptions in the endocrine system, poor ecology, vitamin deficiency, and frequent stress.
Keratomycosis is pityriasis versicolor that affects the upper layer of the epidermis
Types of mycoses in children:
- Keratomycosis - pityriasis versicolor, pityriasis versicolor, nodular trichosporia. The diseases are characterized by the absence of an inflammatory process and minor damage to the upper layers of the epidermis.
- Dermatophytosis – trichophytosis, microsporia. Pathological processes penetrate deep into the epidermis and affect nails and hair.
- Candidiasis - occurs when the number of fungi of the genus Candida increases. The pathology affects the skin and mucous membranes, accompanied by the appearance of a cheesy coating with a sour odor and numerous small white pimples.
- Deep mycoses – chromomycosis, histoplasmosis, blastomycosis. Fungi penetrate deep into the skin, affecting nearby tissues and internal organs.

Candidiasis affects the mucous membranes
A fungal rash looks like spots of different diameters and shapes; they can be pink or yellowish-brown, their surface is flaky and covered with scales.
READ ALSO: Top 10 strips for blackheads on the face and nose: black and other options to choose from with price and reviews
Non-infectious types of rash
Non-infectious rashes occur due to improper care and may indicate disturbances in the functioning of internal organs.

With toxic erythema, spots appear on different parts of the skin caused by a change in environment
The main types of rashes of non-infectious origin:
- Neonatal acne – numerous yellow or white pimples on the forehead, cheeks, and around the nose are present at birth or appear during the first 6 months of a child’s life. The pathology occurs under the influence of the hormone estrogen, due to the active work of the sex glands, and does not require specific treatment.
- Erythema toxicum is a reaction of a newborn’s skin to a new environment. Groups of spots of different sizes appear on the chest, buttocks, and in the bends of the limbs, yellowish-gray blisters, and the skin in the areas of the rash is dense. In a localized form, the rash disappears within 2–4 days; in a generalized and widespread form, it can persist for up to 20 days, with an increase in temperature, and the baby becomes restless due to severe itching.
- Milia - small white nodules localized on the face. The disease develops 7–14 days after the birth of the child due to blockage of the sebaceous glands.
- Pilar (follicular) keratosis is a chronic disease that occurs due to a disruption in the process of desquamation and keratinization of epithelial cells. Small rough nodules appear in the locations of the hair follicles, most often the disease goes away with the onset of puberty.
- Diaper dermatitis is a consequence of improper skin care for a child. Redness, blisters, and peeling appear in the groin area, in the folds of the skin, and in places of friction with clothing.
- Seborrheic dermatitis - develops in newborns and adolescents when the sebaceous glands are disrupted; the problem arises due to overheating, excessive sweating, dietary errors, and stress. Symptoms: the skin swells, turns red, peels, there is severe itching and burning, the condition and appearance of the hair worsens, but yellow crusts appear on the head.
- Miliaria - skin irritation due to increased sweating, failure to comply with hygiene standards, small bubbles of pink, pearlescent, white, flesh color appear.
Allergic skin diseases
Allergic dermatoses are quite often detected in children; they develop against the background of infectious pathologies, poor nutrition; allergens can be foods, household chemicals, pollen, animal hair, dust, and medications. Allergies are often inherited.

Atopic dermatitis - allergic pathology
List of dermatoses of allergic origin:
- Contact dermatitis - severe irritation occurs after contact with household chemicals, some plants, intolerance to sunlight, low temperatures. Usually blisters and red spots disappear on their own when exposure to allergens stops.
- Diathesis – red, rough spots appear on the cheeks; the disease occurs in infants under one year of age if the mother consumes prohibited foods; in older children, such rashes indicate a food allergy.
- Atopic dermatitis is the most common type of allergic childhood pathology and is often hereditary. A polymorphic rash in the form of red spots of irregular shape, pustules, vesicles appears in various areas, but most often on the face, head, in places where joints are bent, and in folds. Symptoms are severe itching, redness of the skin, vascular network, increased dryness of the skin, thickening of all layers of the epidermis, disturbance of the psycho-emotional state.
- Toxidermia is an acute inflammation of the skin and mucous membranes that manifests itself under the influence of allergens and is characterized by the appearance of rashes, blisters, and purulent nodules. Irritants can be food, medications, toxic fumes. Additional symptoms are fever, chills, itching, inflamed areas hurt, and sometimes vomiting and nausea are observed.
- Urticaria - occurs after contact with plants, insect bites, consumption of allergenic foods, during treatment with antibiotics, against the background of infectious diseases. The blisters are localized in different areas of the skin and mucous membranes, and the child is bothered by severe itching.
- Eczema is often a consequence of severe stress, the disease is recurrent in nature, and aggravation is noted in winter.
Rash as a manifestation of diseases of internal organs
Often, a rash indicates a disruption in the functioning of internal organs; rashes appear if a large number of toxins accumulate in the body, some of them are excreted through the pores. Most often, skin manifestations occur in diseases of the gastrointestinal tract, liver, intestines, and hematological pathologies.
READ ALSO: Purulent acne appeared after depilation, what to do?

Acne on a child's face appears due to problems with the intestines.
Description of rashes in various diseases
| Types of diseases | Characteristics of rashes |
| Bowel diseases | Dermatitis, pimples, acne, peeling - usually the rashes are localized on the face. |
| Liver diseases | Single red spots, pustules, small pink rashes all over the body, the skin on the palms becomes marbled. Liver plaques are flat, yellowish lumps located on the limbs, eyelids, and armpits. |
| Blood diseases | Purpura - numerous small bruises throughout the body. Small nodules on the lower limbs and buttocks. |
| Kidney diseases | Increased dryness, yellowing of the skin, age spots, itchy rash all over the body. |
Types, forms, stages of streptococcal pyoderma
The names “streptoderma” and “streptococcal pyoderma” refer to the same disease.
More precisely, streptoderma is one of the varieties of pyoderma - a large group of dermatological purulent diseases. Read more about what pyoderma is and how to treat it here.
The classification of the disease is based on different signs and manifestations. Considering the depth of damage to the skin, the disease is divided into:
- Superficial (impetigo) - when the skin is not deeply affected, at the level of the epidermis. Read here about treatments for impetigo.
- Deep (ecthyma) - the lesion penetrates into the germinal layer of the dermis and even deeper.
Depending on how widespread the rashes are, streptoderma is divided into:
- focal or local (with single formations);
- diffuse – when extensive skin lesions are diagnosed.
Considering how the infection proceeds, it is divided into acute and chronic. Analyzing the nature of the lesions, streptoderma is classified as ulcerative (weeping) or dry.
Depending on the nature of the rash, streptoderma is divided into the following types:
- Streptococcal (contagious) impetigo, which is also called simple streptoderma. This type of infection is more common than others. The rashes are often single, localized on the face, feet, hands, sometimes on the torso and scalp. Children often have streptoderma in the nose and lips. Streptococcal impetigo can be quickly cured if the development of the disease is noticed at an early stage. Lack of treatment and necessary hygiene complicate and prolong the course of the disease.
- Bullous impetigo, also known as streptoderma bullosa. This type of disease is more severe. The most common areas of damage are the legs, feet, and hands. Bullae (large blisters) are formed there, filled with liquid purulent-serous contents. Open erosions appear in place of burst bullae. Bullous impetigo is always accompanied by high fever, inflammation of the lymph nodes, and general malaise.
- Slit impetigo, also called streptococcal impetigo. The location is in the corners of the mouth, much less often in the folds of the wings of the nose or in the corners of the eyes. With adequate treatment, seizures go away quickly enough, but relapses may occur. The main reasons are vitamin deficiency, caries, lack or lack of personal hygiene.
- Streptococcal diaper rash, another name for which is intertriginous streptoderma. The lesion is localized in the skin folds behind the ears, in the groin area, on the genitals, armpits in infants, and in obese people also on the stomach and under the mammary glands. The peculiarity of this type of streptoderma is that bacterial damage occurs against the background of ordinary diaper rash. The bursting bubbles form a continuous wet area. The disease occurs with high fever.
- Tourniol is also called streptoderma or impetigo of the nail folds. The skin around the fingernails becomes inflamed, swollen, and covered with phlyctenes, which then turn into erosions. Pathology occurs as a result of the pathogen entering the affected areas of the skin - where there are abrasions, wounds, hangnails.
- Streptococcal ecthyma vulgaris is a severe form of streptoderma, which affects the deep subcutaneous layers. Ecthyma is characterized by ulcers and erosions that do not heal for a long time. Scars then form on these areas. The formations are localized on the child’s bottom, on the legs, and less often on the skin of the hands and body. The course of the disease is severe and protracted.
- Erythematosquamous (dry) streptoderma. The skin of the face is affected - formations in the form of flaky spots appear on the cheeks, on the chin, but there are no weeping blisters.
- Lichen simplex is considered a dry abortive form of the disease. Much more common in children. It is expressed in the formation of flaky spots on the face, sometimes on the body and on the limbs. These areas undergo depigmentation when exposed to sunlight.
- Papuloerosive streptoderma is also known as diaper dermatitis. It affects infants, including newborns. Irritation under the influence of feces favors the penetration of streptococcus and its reproduction. The disease affects the buttocks, thighs, and perineal area.
Streptoderma in children, how it begins
It begins immediately after contact with the infection, after this time the incubation period begins, and during streptoderma it lasts for almost a week. Much depends on your child’s immunity, so I always advise strengthening it using many means, including traditional medicine.
Streptoderma is transmitted from person to person much faster than chickenpox, and the pathogens also begin to act immediately. The virus appears as a lesion on the child's skin. Purulent rashes can appear anywhere, on the child’s body, on the face, in the nose, in the throat and more.
- Bulleznaya. It looks like pimples or small blisters that appear a day after the red dot appears on the body. Then a purulent drop appears in the pimple. They burst easily, and in this place a crust appears, resembling growths of scales, a scab.
- Nonbulous. This form is much more difficult to treat than the previous one. In this case, large blisters with pus develop, the child’s condition becomes serious, and after the growth is rejected, irregularities remain on the body. Most often, such streptoderma appears on the limbs, arms and legs.
- Chronic. It manifests itself with incorrect and illiterate treatment.
Diagnostics
An experienced doctor will be able to diagnose streptoderma based on external signs and by examining the patient. It is important to distinguish the infection from other diseases with similar initial symptoms.
In cases where doubts arise and it is necessary to confirm the diagnosis with laboratory tests, the following may be prescribed:
- blood tests - general, biochemical, sometimes for HIV infection;
- urine test (general);
- bacteriological culture of liquid from affected areas to determine the causative agent of the disease and its sensitivity to various antibiotics;
- examination of stool for the presence of worm eggs.
The decision on the need for such tests is made by the attending physician. It is better to undergo additional examinations to make a correct diagnosis and begin adequate treatment.
Symptoms of streptoderma
Streptoderma in children occurs with severe symptoms:
- temperature rise to 39°C;
- intoxication;
- enlarged lymph nodes.
The condition of the skin differs depending on the form of the disease:
- Superficial. First, red spots appear on the skin. After 2-3 days they transform into blisters with a cloudy liquid inside. The blisters increase to 2 cm in diameter, then burst. In their place, yellow crusts form. Subsequently, the skin in this place heals, and the disease spreads further.
- Dry. This form is more common in boys. White and pink spots up to 5 cm in diameter form on the skin. They are located on the face, neck, ears, arms and legs, and are gradually covered with a scab. After healing, scars may remain. These areas remain lightened and do not tan under the sun.
- Streptococcal infection. The disease affects the corners of the mouth and occurs when there is a lack of vitamin B. Microcracks appear on the skin, which hurt and bleed. Then they transform into pustules that become crusty. It hurts the child to open his mouth, eating becomes difficult. Less commonly, streptococcal seizures occur in the corners of the nose or eyes.
- Felon. If streptococcus affects the periungual ridges, panaritium occurs. It is more common in children who are accustomed to biting their nails. Over time, the ulcers open up.
- Streptococcal diaper rash. This form of the disease is typical for infants. Blisters form in the folds of the skin. They gradually merge. If they are opened, pink, weeping surfaces are exposed.
Knowing how streptoderma begins in children, parents will be able to contact a dermatologist in time and begin treatment. If you delay going to the doctor, the disease becomes chronic, and achieving a complete cure becomes very difficult.
How is it different from other diseases?
Even not every doctor will be able to make the correct diagnosis and differentiate streptoderma from other diseases from the first examination.
The problem is that this infection is very “many-faced”; it has many varieties that are localized on different parts of the body.
Parents can all the more easily confuse the manifestations of streptococcal pyoderma with other infectious and dermatological diseases - herpes, chickenpox, eczema, urticaria, atopic dermatitis, allergies.
The general symptoms are similar for many diseases, but each of them has special, characteristic signs, which are used to make a diagnosis.
In skin diseases, the main symptom is rashes, which differ in their location and appearance:
- For example, a herpetic rash is distinguished by pain, while a chickenpox rash is distinguished by the presence of rashes of different stages at the same time - from pimples to crusty dried blisters.
- With streptoderma, there are no catarrhal symptoms - no runny nose or cough. The rash is also different from skin lesions associated with other diseases. With streptococcal infection, the contents of the blisters are clear, not cloudy.
- Seizures with streptoderma differ from similar formations with herpes in that the conflicts quickly open, and then cracks form in the corners of the mouth. Herpes blisters last longer, but then no cracks form.
Such nuances distinguish streptoderma from other, at first glance, similar diseases. But only an experienced doctor can correctly differentiate the infection.
If you are interested in how to quickly treat a cold on your lip, read our post and find out.
Instructions for using Belogent ointment, its cost and consumer reviews of the drug are presented in this material. Find out more!
Treatment methods
Due to the fact that streptoderma is caused by pathogenic microorganisms in the form of streptococcal bacteria, the disease in infants and older children is treated with antibiotics. In addition, emollient ointments, vitamin preparations, local antiseptics and some other agents are used.
Ointments
Ointments are used among children as prescribed by a doctor. Medicines in this form of release provide effective disposal of pathogenic microflora on the skin, which promotes a speedy recovery.
Names of popular ointments for the treatment of streptoderma:
- Baneocin;
- Fucidin;
- Levomekol;
- Akriderm GK;
- Zinc;
- Acyclovir;
- Tetracycline ointment and others.
The affected areas on the child’s body with streptoderma should be smeared according to the scheme prescribed by the doctor. Typically, the course of treatment with antibacterial agents lasts 7-10 days, but sometimes treatment has a longer duration, which depends on the severity of the disease in a particular patient. When it comes to treating infants, independent use of any medications is strictly prohibited. Before starting therapy, you should definitely show the child to a specialist.

If the rash is located on the lips, on the eyelid, or in the corners of the mouth, ointments should be used with extreme caution. It is important to ensure that the medicine does not get on the mucous membranes.
Medicines for internal use
Sometimes it can be quite difficult to cure streptoderma using only ointments. This may apply, for example, to situations where the rash is hidden under the hair on the head or the course of the pathology is complicated. In such cases, doctors prescribe therapy with oral antibiotics.
Antibacterial agents for internal use:
- Sumamed;
- Amoxiclav;
- Flemoxin Solutab;
- Augmentin;
- Suprax and others.
Any antibacterial drugs must be used according to a strict regimen with clear dosages. Violation of the instructions can provoke a relapse of the disease and a poor therapeutic effect. In addition, improper use of antibiotics often leads to the development of side effects.
You may be interested in: Allergies in newborn babies
Antiseptic solutions
Modern pharmacology offers a wide selection of disinfecting solutions for local treatment of rashes for various skin pathologies. Their use is convenient and, most importantly, safe.
Treatment of streptoderma involves opening the blisters and then treating them with antiseptics and antibacterial ointments. Solutions for local disinfection include:
- Hydrogen peroxide;
- Brilliant green (zelenka);
- Fukortsin;
- Salicylic alcohol.
These drugs are used exclusively for external use. In this case, it is necessary to capture not only the diseased area, but also several millimeters of healthy skin. How many times should I smear the dermis in the affected areas? Repeated treatment is carried out 2-3 times a day.
When applying antiseptic to the skin, the child may experience pain and burning. After the solution dries, these sensations go away.
Treatment with traditional methods
At home, treatment of streptoderma in children can be carried out using some folk recipes.

Let's look at a few of them:
- Garlic juice. This is a simple and safe method to get rid of rashes. Garlic has been proven to be an excellent natural antibiotic. To treat blisters, it is necessary to lubricate the affected areas of the skin with juice 3-4 times throughout the day.
- Potassium permanganate solution. To prepare a disinfectant, you need to dissolve several granules of pink powder in boiled water and treat the wounds on the child’s body with this product. This medicine will quickly eliminate pathogenic bacteria.
- Chamomile. The plant has an analgesic, wound-healing and disinfectant effect. Chamomile decoction will help get rid of the sore. To prepare it, you should brew a tablespoon of the plant with a glass of boiling water and let the product brew for 1.5-2 hours. Rinse the wounds with the resulting medicine.
- Calendula flowers. Brew a tablespoon of the plant with a glass of boiling water and leave the medicine for several hours. Treat the rash areas with the resulting product.
- Pomegranate juice with honey helps eliminate streptoderma in a child. To do this, the products must be mixed in equal proportions and stored in the refrigerator. The affected areas should be lubricated with this medicine 3-4 times a day.
Reviews from parents indicate the good effectiveness of natural treatment, but any procedures should be done only after consultation with a doctor. The fact is that some foods can cause allergies in a child. The doctor will help you choose safe products and give advice on their use in combination with drug treatment.
Treatment of streptoderma in children and adults at home
How long will it take to treat streptoderma? With proper treatment and compliance with certain rules of behavior, the disease goes away in a week, maximum 10 days. Treatment of complicated forms of the disease may take more than 2 weeks.
Those who want to heal themselves put themselves at risk. You cannot prescribe medications for yourself after reading advice on the Internet or trusting the experience of friends and relatives.
The fight against streptoderma involves a combination of general and local therapy. It is also necessary to adhere to basic hygiene rules:
- you should not wash, especially in the first days of illness, because water contributes to the spread of rashes;
- clean areas of the skin should be wiped with a cotton pad soaked in a decoction of herbs (chamomile, calendula, string);
- provide the patient with separate dishes and a towel;
- Wash bed linen separately, it is better to boil it and change it often;
- observe food restrictions - give up sweets and baked goods, spicy and fried foods. A healthy diet will include dairy products, lemons, fresh berries, carrots, cabbage, garlic, and herbs.
Local treatment is effective for mild forms of streptoderma. The affected areas are treated with antiseptic solutions:
- Fukortsin;
- Miramistin;
- hydrogen peroxide;
- alcohol solution of Chlorhexidine;
- boric acid;
- salicylic alcohol;
- brilliant green.
Several times a day, an antiseptic is applied to the sores, covering the area around them. When the product dries, treat the affected area with ointment:
- Erythromycin;
- Tetracycline;
- Ichthyol ointment;
- Levomykol;
- salicylic-zinc paste;
- Hyoxyzone;
- Baneocin.
Ointments and creams with hormones have a strong effect, but they are prescribed with caution to adults, as they have many side effects.
Such drugs are prescribed to children only in special cases. For streptoderma, Akriderm, Triderm, Lorinden S are used.
If the rashes are located in the hair on the head, then you first need to soften the crusts, for example, using salicylic petroleum jelly, remove them, and then apply lotions using antiseptics and smear the affected areas with bactericidal ointments.
For streptoderma in the mouth, Metrogyl-Denta gel and applications based on Stomatidin are used.
Sulfur is used as a homeopathic remedy for skin diseases. In many cases, antibiotics cannot be avoided.
Dr. Komarovsky emphasizes that antibacterial agents help effectively fight infection caused by streptococci.
Oral antibiotics are not prescribed to children if there are not many rashes and they can be treated with local drugs. But if the disease is severe, you cannot do without taking antibacterial drugs.
Streptoderma is treated with various drugs from the groups of Penicillins, Cephalosporins, Macrolides:
- Amoxiclav;
- Augmentin;
- Amoxicillin;
- Doxycycline;
- Cefazolin;
- Erythromycin;
- Sumamed;
- Clarithromycin.
The use of Acyclovir is not advisable, since this drug has an antiviral effect, and streptococci that cause the infection are bacteria.
Complex therapy for streptoderma includes the use of various medications:
- In order not to suffer from itching, antihistamines are prescribed: Diazolin, Zyrtec, Diphenhydramine, Suprastin, Claritin, Tavegil.
- To restore damaged intestinal microflora, you should drink one of these drugs: Linex, Duphalac, Acipol, Hilak-Forte.
- To strengthen the body and help it recover, it is recommended to take vitamin complexes - Vitrum, Complivit, Supradin, Multitabs, Alphabet.
- In some cases, the prescription of immunomodulators is required - Anaferon, Arbidol, IRS 19, Cycloferon, Viferon, Pyrogenal.
Folk remedies are used as an addition to the main therapy.
You can disinfect and heal wounds with decoctions of sage, chamomile, oak bark, and a series of lotions and applications.
Strengthening the immune system is helped by taking echinacea tincture, herbal teas with lemon, ginger and honey, infusion of rose hips, berries pureed with sugar - viburnum, lingonberries, cranberries.
How does streptoderma begin in children?
The most important thing in any disease is to recognize the first signs in time, how the disease begins, in this case streptoderma, then you need to get information on how to treat the child, what tablets, ointments and other types of drugs to give, you may need treatment with traditional medicine.
Of course, if you have any symptoms or rashes, you should contact your pediatrician, who will diagnose the disease, prescribe appropriate treatment and give recommendations. If you don’t have such an opportunity, I suggest you take note of my advice from personal experience.
First you need to understand what this unpleasant disease looks like in the photo, find out in detail how it begins, the reasons for its appearance, and, of course, how to cure streptoderma in a child.
How and with what to treat newborns and infants
The danger of streptoderma in infants is that it can have autoimmune consequences . Therefore, it is necessary to treat the infection even in infants.
Therapy should begin with the use of local drugs - treating lesions with antiseptics and ointments. The doctor will prescribe the most gentle means acceptable in the treatment of children in the first months of life.
If this is not enough, children are prescribed antibiotics. That is, the treatment regimen does not differ from the treatment used in older children and adolescents.
The difference is in the dosage and in the limitation of the number of drugs allowed for the treatment of infants. Plus – strict control of all prescriptions and procedures by the attending physician.
Parents must carefully follow the rules for caring for their child during this period:
- do not bathe the baby, wipe the skin with a napkin soaked in herbal decoction;
- dress the baby in clothes made from breathable natural fabrics;
- use diapers as little as possible and keep the baby’s body clean after bowel movements;
- treat objects used by the child with antiseptics.
A specialist will talk about the treatment of streptoderma in children in this video:
Streptoderma in children in the picture
Photos of these sores on the body are not entirely pleasant, but you should look and evaluate the similarity. Perhaps you are not experiencing streptoderma, but a common allergy to sweets. Sometimes it is precisely this allergic reaction that manifests itself in purulent abscesses.

You can read more detailed information in my article entitled – sweet allergy in children.

And this is what dry streptoderma looks like in children in the photo.
How to quickly cure women during pregnancy
Is it necessary to treat streptoderma in pregnant women? There is an opinion that it’s not worth it, the disease will go away on its own in a couple of weeks. But one cannot ignore the fact that there is a risk of infection of the fetus.
Therefore, therapy for streptoderma is necessary, but only gentle and absolutely safe for the woman herself and her unborn child.
The doctor must select suitable antiseptics and antibacterial agents in the form of creams and ointments. On average, the course of treatment takes from 7 to 10 days.
If local therapy is not effective, antibiotics are prescribed. These can be tablets or injections. The safest drugs are those from the penicillin group.
In addition to taking prescribed medications, pregnant women need to adhere to simple but important recommendations:
- Showering is prohibited during the treatment period.
- Be sure to wash your hands after applying the antibacterial agent to the affected areas.
- You cannot peel off the scabs covering the ulcers; they will fall off on their own.
- The localized lesions can be covered with sterile bandages.
Where does streptoderma come from in children?
Streptococci are bacteria that can be found on the skin of any person. They are so small that they can only be seen under a powerful microscope. Normally, bacteria live on the body without causing harm to the body. However, a small inflammation is enough, and they easily penetrate into the layers of the epidermis - through scratches, wounds, cuts, becoming sources of serious illness in children.

Not all children become infected with the disease. Only those who do not have good immunity are at risk. An important factor is compliance with sanitary and hygienic standards. Irregular changing of diapers, poorly washed linen or clothes, infrequent hand washing - ordinary household little things “help” bacteria get under the skin and weaken the child’s fragile health.
The bacterium can enter the body even through minor injuries, and the incubation period of the disease lasts from 7 to 10 days. At this time, the chances that the baby will become infected himself or infect other children through:
- airborne droplets (from sneezing, coughing);
- contact path (with tactile touches);
- household route (when infected and healthy children pick up the same toy or object).
Streptoderma begins with the appearance of purulent swellings on the body. Failure to seek medical help in a timely manner can have serious consequences. Non-healing wounds form on the skin, and in the most difficult situations the development of microbial eczema is provoked. The infection also causes complications on internal organs (in the form of meningitis, otitis, sinusitis, pneumonia, endocarditis, myocarditis).

Consequences and complications
The danger of streptoderma is that if the disease is diagnosed untimely and becomes chronic, the consequences can be very serious:
- possible autoimmune diseases;
- there is a high risk of damage to the cardiovascular system, kidneys and other internal organs;
- the development of allergic dermatitis is possible;
- there is a risk of tissue abscess;
- possible diseases - erysipelas, rheumatism, sepsis, eczema of microbial origin, glomerulonephritis, scarlet fever;
- there is a danger of cosmetic defects – scars and cicatrices.
Any of these diseases poses a health hazard and requires timely treatment.
In this article you will find a description of the symptoms and causes of development, as well as photos of allergic dermatitis in adults, and ways to eliminate the problem.
Treatment methods for candidal stomatitis in adults are discussed in this material.
Photo of herpes on the toes - here: https://udermatologa.com/zabol/gerp/gerpes-na-paltsah-i-stupnyah-nog-foto-lechenie-simptomy/
Prevention
General preventive measures to prevent infection with streptoderma come down to following simple rules:
- do not forget about basic hygiene - regular hand washing with soap;
- avoid using other people's things - combs, towels, cosmetics, toys;
- lead a healthy lifestyle with moderate physical activity, walks, a balanced diet, and hardening procedures;
- avoid contact with people with streptoderma;
- treat all skin damage, even minor abrasions and scratches, with antiseptics;
- At the first suspicion of infection, immediately consult a doctor.
Streptoderma is a contagious disease; sick people should be urgently isolated from the community. Anyone who has been in contact with the patient is subject to a 10-day quarantine.
Family members should take precautions, disinfect premises more often, and wash their hands. The patient needs to be provided with separate dishes, bedding and towels.









