Children drink milk, you will be healthy! Of course, milk contains calcium, minerals, vitamins, and is rich in protein and fat. But what to do when this drink brings harm rather than health to children? And will this go away with age?
According to statistics, about 10% of children under one year of age are allergic to dairy products. It is known that allergy is a response to the introduction of a foreign protein-antigen into the body. There are about 25 such antigens in cow's milk. The most active in this regard are beta-lactoglobulin, serum albumin, alpha-lactoglobulin, and casein.
Protein in its structure resembles a chain, the links of which are amino acids. Once in the stomach and intestines, under the influence of enzymes, the chain breaks down into individual elements, which are easily absorbed by the body.
In children, the digestive system is completely immature, there may not be enough enzymes, and then this chain is not completely destroyed, but contains several links at once. Such structures cannot be absorbed in the intestines, and an immune response occurs, which manifests itself in the form of allergies.
- A true milk allergy is if a child with an immature enzymatic system drinks a small amount of milk (or receives it through breast milk) and his body cannot cope with the protein load.
- Pseudo-allergy - there are enough enzymes and they work well, however, the child drank so much milk that the digestive system could not cope. Excessive protein load on a normally functioning body will also cause allergies. In this case, the allergy is not due to the nature of the product, but due to its quantity
A distinction is made between milk protein intolerance and cow's milk protein allergy. Intolerance is difficulty digesting milk and the immune system is not involved, while allergy is a reaction of the immune system to a foreign protein.
Why do allergies occur?
In some sources, milk allergy is indicated as an inadequate reaction of the body only to milk protein, in others to milk sugar - lactose (see lactase deficiency). Both will be right, since when consuming dairy products, an allergic reaction can be triggered by both milk protein and lactose.
For a newborn baby, everything except mother's milk, any mixture, is the roughest food. In infants, the mucous membrane of the digestive tract is loose, immature, not protected by natural microflora, and is easily accessible to allergens. Only by the age of 2 in children do the walls of the stomach and intestines acquire the ability to resist the introduction of pathogenic agents. In cases where:
- Mom herself is prone to allergic reactions
- pregnancy took place in unfavorable environmental conditions - an industrial city, a metropolis, work in a hazardous industry
- there was a pathological course of pregnancy - stress, fetal hypoxia, threats of miscarriage, gestosis during pregnancy, etc.
The risk of developing allergies in a child increases. That is, factors such as heredity, ecology, nutrition, lifestyle, bad habits in the family, health and age of the mother, and the course of pregnancy are considered important.
A sentence or a temporary phenomenon?
The discovery of a milk allergy causes shock among parents, and the first question they ask the allergist is: “Is this allergy forever?” Of course, no allergist will tell you 100% that this will go away. But as practice shows, in most cases, an allergy to dairy products can go away completely up to a year or become less severe. For example, there are often cases when a child suffering from allergies cannot consume milk or products containing milk powder, but may in the future eat fermented milk products (yogurt, cottage cheese, sour cream).
Very often, allergists say that such an allergy to dairy products is associated with the immaturity of the gastrointestinal tract system in children. The gastrointestinal tract fully matures by the age of 3 in children, which means that there is a chance to get rid of allergies by the age of 3 in your child. But, of course, this is all very individual and requires consultation with specialists (allergist, gastroenterologist, pediatrician).
How does a milk allergy manifest?
Since allergens circulate in the blood, any organs and systems can be involved in an allergic reaction. An allergy to cow protein can be aggravated by stress, colds, severe infectious diseases, or poor environmental conditions.
Gastrointestinal disorders
In children under one year of age, this will manifest itself in the form of loose stools. Due to the fact that the digestive organs cannot cope with their duties:
- undigested food residues and curdled milk appear in the stool
- Vomiting may occur, and in young children - frequent and profuse regurgitation (see causes of regurgitation in infants)
Milk proteins are attacked by the body's antibodies, and along with the antigens, the intestinal mucosa is also damaged.
- Therefore, red blood cells may be present in the stool, which is detected only with a special analysis, or streaks of blood visible to the eye. This is a sign of severe allergies.
- Damage to the intestinal mucosa manifests itself as abdominal pain. Young children are often restless, capricious, and cry. This condition must be differentiated from colic (see what to do with colic in a baby). It should be noted that such a reaction will only occur when cow's milk or a fermented milk mixture based on it enters the body. Breast milk itself should not cause allergies (except in extremely rare cases), but the products that the mother eats can.
- In children after a year of constant intake of dairy products, the pain becomes chronic. It is short-term in nature and localized near the navel. Intestinal colic, impaired intestinal motility, and symptoms of colitis may also bother you.
- With any allergic reaction, histamine is released, which, in turn, leads to a response increase in hydrochloric acid in the stomach. This explains pain in children in the epigastric region.
A long-term and persistent milk allergy in a child can cause secondary enzyme deficiency. The absorption of lactose and cereal gluten is reduced (see symptoms of celiac disease, list of gluten-free products), and the production of enzymes by the pancreas is reduced.
The number of bifidobacteria in the intestines also decreases, and they are replaced and multiplied by opportunistic microbes: E. coli, enterococci (see how to treat intestinal dysbiosis, probiotics, Linex analogues). All this adversely affects the child’s well-being.
Skin lesions
The skin is the second organ that suffers greatly from food allergies. The most common symptoms of milk allergy:
- Milk scab
This is the first signal that something is wrong in the baby’s body. Milk scab is more common in pink-cheeked toddlers who are bottle-fed. Of course, infants can also have it, but the cause will not be cow’s milk protein, but another product that the mother consumes. Milk scab, or scientifically gneiss, looks like a crust on a child’s head. The crust itself can be greased with Vaseline or vegetable oil and combed out with a comb.
- Childhood eczema
It most often appears on the cheeks, but can appear on any other parts of the body. First, bubbles appear, then erosion, which produces exudate - a clear liquid. Then the wounds heal, scales and crusts form. Children under 6 months of age suffer.
- Limited atopic dermatitis
Appears under the knees, on the inside of the elbows in the form of plaques covered with scales. The rash may periodically become wet and very itchy (see treatment of atopic dermatitis in children).
- Quincke's edema
Acute allergic reaction to taking a dairy product. It manifests itself as swelling in places with developed subcutaneous tissue - the mucous membrane of the mouth, lips, eyelids, genitals. There is no itching of the skin. If swelling occurs in the laryngeal mucosa, there is a high risk of asphyxia, that is, the child may simply suffocate. This condition is urgent and requires emergency care and the administration of hormonal drugs.
- Urticaria (see symptoms and treatment of urticaria)
It is also an acute reaction, but if it is not widespread, it is not as dangerous as Quincke's edema. Blisters appear with redness around them, which are very itchy and itchy. In appearance, urticaria resembles a nettle burn, which is why it has this name. In this case, taking antihistamines is mandatory (see list of allergy pills for children).
Respiratory system damage
Manifestations from the respiratory system are uncommon and include:
- Sneezing, allergic rhinitis (see how to treat allergic rhinitis)
- Difficulty breathing, wheezing with the risk of developing laryngospasm. This is an emergency condition that involves swelling of the laryngeal ligaments. In this case, it is impossible to take a breath and the child begins to choke.
- Bronchial asthma - an allergy to cow's milk protein is one of the triggers for its development.
Symptoms
It is necessary to distinguish between an allergy to cow protein and its intolerance. In the first case, the body sees it as a foreign element and begins to defend itself, and in the second, the problem is poor digestibility of dairy products. The reaction in children to cow's milk protein manifests itself in skin rashes on the face, disorders of the digestive and respiratory systems.
Skin symptoms:
- peeling of the skin;
- the appearance of milk scab, eczema;
- sensation of skin itching;
- rash (urticaria);
- large red spots on the surfaces of the skin of the face and chest - atopic dermatitis;
- rapidly increasing swelling in the neck and head area - Quincke's edema.
With regard to digestive disorders, an allergy to cow's milk in children manifests itself:
- intestinal disorders - colic, constipation, diarrhea, flatulence;
- abdominal pain;
- nausea, vomiting.
The respiratory tract responds to cow protein:
- nasal congestion;
- cough;
- difficult, wheezing breathing;
- runny nose;
- wheezing.
All these reactions occur immediately when protein enters the child’s body and manifest themselves both individually and in combination. A delayed reaction may be diarrhea or itchy skin that appears after a few days.
Attention should be paid to such alarming symptoms as angioedema and rash, the spread of which occurs rapidly. Such conditions are life-threatening for children and require urgent medical attention.
Another factor that causes parents to fear for the health and life of the baby is the presence of a barking cough, dry wheezing, or whistling breathing. Medical assistance required.
An allergy to milk in a child manifests itself at an early age, often before one year. With proper treatment, it disappears by about 5 years, and only occasionally persists for life.
If the disease does not go away by this age, problems with the allergy turning into other forms of the disease, especially dangerous bronchial asthma, cannot be ruled out.
Allergy to goat's milk in children is much less common. Its signs include:
- rash, skin eczema;
- inflammation of the eyes, nasal mucosa;
- itching in the mouth (rare);
- hard breath.
The specific taste and smell that goat's milk has causes aversion in many children, and it is difficult to feed food based on it. Experts believe that the body senses that this product can become a potential allergen, so you should not feed your child food containing such milk if he refuses. The cause of an allergy to goat's milk is considered to be a hereditary factor, the child's weak immunity.
How to determine that this is a reaction to milk?
The doctor collects anamnesis - the presence of allergic manifestations, atopic dermatitis, chronic diarrhea, poor weight gain, anemia, etc.
Tests - to exclude other diseases and allergies to other products from milk intolerance and protein allergies, the doctor will order tests: coprogram, stool for dysbiosis, blood test for allergens (IgE immunoglobulins to cow's milk protein, etc.), skin test test.
How to distinguish a milk protein allergy from lactase deficiency? Symptoms can be very similar: colic, bloating, regurgitation, diarrhea. The baby's stool is watery, foamy, and sometimes may be green, more than 8–10 times a day. There is also a combination of these two pathologies.
In lactase deficiency, the cause of all these unpleasant symptoms is a lack of the enzyme lactase. Its function is to break down the disaccharide lactose into simple carbohydrates for absorption in the intestines. If there is not enough lactase, then lactose is not broken down and is retained in the intestines. This leads to an increase in osmotic pressure and fluid influx. This is how diarrhea, flatulence and other symptoms appear.
Test for lactase deficiency
In order to distinguish lactase deficiency from protein allergy, your doctor will advise you to conduct a simple test. It consists of a lactose-free diet for several days:
- if the child is bottle-fed, transfer him to a lactose-free formula
- if breastfed, the mother follows a dairy-free diet
- if the child is older, they do not give milk and dairy products
If there are no symptoms in the near future, it is believed that lactase deficiency is to blame. Why not a protein allergy? Because several days will not be enough to remove the allergen from the body and the symptoms will not stop so quickly.
In addition, milk allergies are more common in young children, tending to disappear by the age of three. And lactase deficiency can be not only from birth, but also acquired. Usually it happens after a child has had intestinal giardiasis or rotavirus infection. In such cases, it is easily eliminated by diet and goes away quickly.
Cause and symptoms
There are several reasons why an allergy to dairy products may be detected. First of all, it is heredity. If one of the baby’s parents suffers from this disease, then the child has a predisposition to this disease.
Formula-fed babies also have increased sensitivity to milk. Infants usually react to cow's milk. For breastfeeding, much less often.
An allergic reaction to breast milk may be caused by the fact that during pregnancy a woman consumed cow's milk and casein, which is part of it, could penetrate the placenta, and then into the bloodstream of the fetus.
If the mother eats foods that can cause an allergic reaction, the likelihood of the baby being sensitive to them increases significantly . Therefore, a woman who is breastfeeding a child should exclude seafood, coffee, chocolate, citrus fruits, honey, nuts and other equally dangerous foods from her diet.
As a rule, a list of permitted and non-recommended products is offered in the maternity hospital.

What to do if your baby is allergic to milk?
Mother's milk is the ideal nutrition for a baby! It is not only easy to digest, it itself contains the necessary enzymes that are activated in the baby’s stomach and help him easily absorb food. Pediatricians advise feeding a child with allergies with breast milk for as long as possible, following a hypoallergenic diet.
Products that contain milk or even traces of milk are excluded: cream, condensed milk, ice cream, chocolate, dry soups, butter, store-bought pastries, powdered milk or powdered cream.
If a breastfed baby develops an allergy to milk, the nursing mother should change her diet (see what a nursing mother can eat). According to different sources of whole milk, a nursing woman can drink from 100 ml to 400 ml per day, but if the child has allergies, it should be abandoned completely; if the allergy is not pronounced, replace it with kefir, fermented baked milk, yogurt, cottage cheese. Only after 2-4 weeks the baby’s condition will improve. If the condition does not improve and a milk allergy is confirmed, then some pediatricians recommend transferring the child to a mixture of deep protein hydrolysis.
As for goat's milk, if you are allergic to cow's milk, intolerance to goat's milk protein is also possible (see why both cow's and goat's milk is harmful for children under one year old). If the baby has a severe allergy to protein, then in addition to milk, eggs, fish, and nuts should also be excluded from the mother’s diet.
If a child has milk intolerance, this does not mean that fermented milk products need to be excluded from the baby’s diet. Feeding such children with fermented milk products should also be done very carefully; you can try to start at 7 months with kefir or homemade yogurt, both from cow's and goat's milk. After 9–10, you can try to introduce cottage cheese (see how to properly introduce complementary foods to a child), after a year, eggs, fish.
Why shouldn't fermented milk products cause allergies? When processing milk, fermented milk products undergo hydrolysis (splitting), milk protein, during fermentation, breaks down into amino acids (simple compounds), the digestibility of which is faster and easier, and allergens remain in very low concentrations.
If you are intolerant to milk, kefir and other fermented milk products do not cause gastrointestinal disorders, bloating, urticaria, etc. However, you should also be careful with them.
How to make cottage cheese yourself?
Store-bought cottage cheese can be given to a child only with special labeling “for children”, but since they can also cause allergies due to the presence of various additives, it is better to make it yourself. Add a tablespoon of sour cream to a glass of milk and leave at room temperature for several hours. Then pour the slightly sour milk into a saucepan and heat over low heat. The process will separate the curds from the whey. It needs to be collected with a spoon or strained, transferred to a piece of gauze, and allowed to drain excess liquid, then squeeze it out. The curd is ready to eat. This product is perishable, so storing it in the refrigerator for more than a day is not recommended.
Types of mixtures and recommendations
The formula for the child should be selected by the treating specialist. Especially if the baby is allergic to cow's milk proteins. The doctor creates an individual hypoallergenic formula or simply helps you choose the brand and composition. General recommendations are also discussed here.
Soy-based mixtures

Soy infant formulas should not be used before six months of age.
The reason is the high content of phytoestrogens in soy. These are compounds that mimic the effects of the female hormonal estrogen and pose a risk to the health and growth of the baby.
Even at older ages, such as 3 years, consult a doctor before purchasing soy milk.
There is also cross-reactivity between milk protein and soy protein. Therefore, some patients with cow protein intolerance have problems with soy.
Goat milk based formulas
Goat milk proteins are better absorbed. Therefore, the gastric mucosa is less irritated. And it processes incoming food faster. In 2020, mothers began to use this mixture very often for their children.
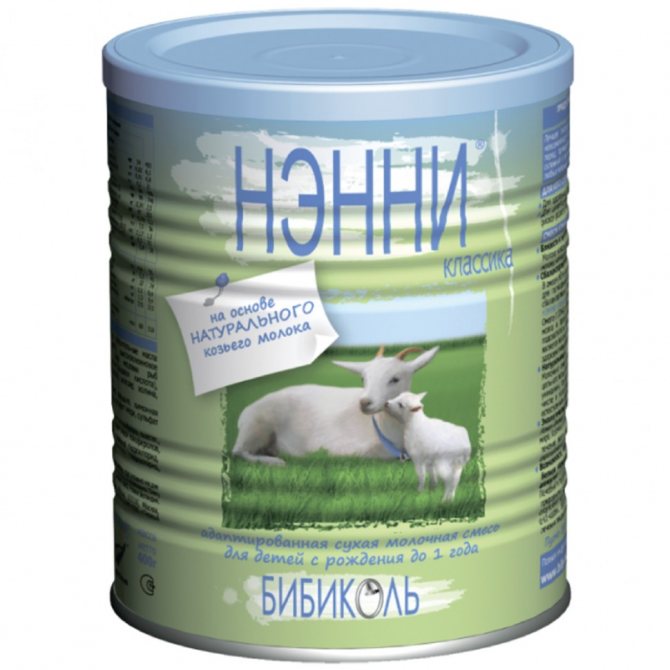
However, although the proteins of goat and cow milk are different, both types are foreign to the baby’s body. Therefore, you may or may not have a goat allergy. Need to try.
In general, goat milk formulas are of better quality. Their cost is higher.

Popular mixtures recommended by experts
Doctors recommend the following brands:
- Nanny. Composition based on goat's milk. It is not suitable for all patients, as it may also lead to a reaction. If it is not there, the allergy will disappear in 1-2 weeks.
- Neocate. Suitable for infants with minor allergic reactions.
- Nutrilon Pepti Allergy. Mixture with highly hydrolyzed cow's milk proteins. Suitable for babies with moderate milk intolerance. The mixture is selected in accordance with the recommendations of the allergist. By the way, doctors recommend Russian-made baby products.
To check if the mixture is suitable, it is better to give the child 1-2 teaspoons. Wait 2-5 hours. There should be no reaction to the correct composition.
What to do if a baby is allergic to milk?
Most modern adapted formulas are made on the basis of cow's milk, so it is recommended to either replace the mixture with another one based on goat's milk, or use hydrolysates for 6 months. Then you can try to change the mixture to a regular one; if the symptoms return, then return to hydrolyzed mixtures and the introduction of dairy products is postponed for another six months.
Mixtures based on goat milk are presented under the names “Nanny” and “Kozochka”. They are well tolerated by children, but are much more expensive than regular formulas. It is worth remembering that changing the formula is not a guaranteed solution to the problem, because a reaction may also occur to goat’s milk.
Hydrolyzed mixtures are foods in which proteins are broken down into dipeptides. They are easily digestible and usually do not contain lactose.
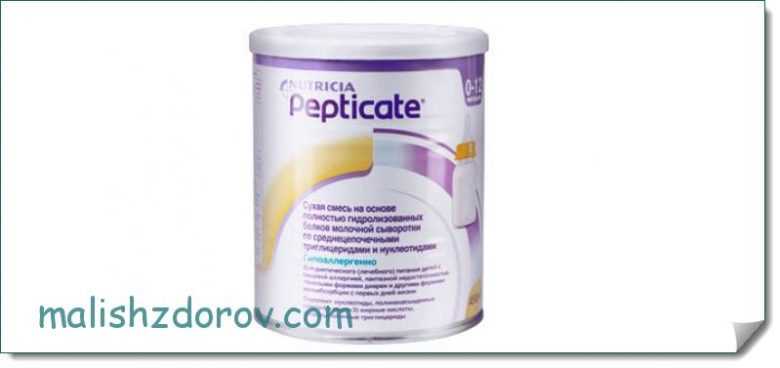
- The market includes “Frisopep AS”, “Pepticate”, “Frisopep”, “Alfare”, “Pregestimil”, “Nutrilak Peptidi SCT”, “Nutrilon Pepti TSC”. Their foreign analogues “Vivonex”, “Vital”, and “Critacare” are used for severe manifestations of allergies to cow protein.
- To prevent allergies in children with a high risk of their occurrence, mixtures with partial protein hydrolysis are suitable: “Nutrilon GA 1 and GA 2”, “NAS GA1 and GA 2”
- For milk intolerance and to prevent the development of allergies: “HiPP GA 1 and GA 2”, “Nutrilak GA”, “Humana GA 1 and GA 2”.
Treatment
What should parents do if they detect negative manifestations in their child? First of all, the baby should be shown to a doctor. The specialist will prescribe the necessary tests and conduct a comprehensive examination to distinguish true allergies from false ones and diseases such as lactase deficiency.
Diet
If a breastfed baby has been diagnosed with milk intolerance, the mother should exclude all foods containing whole milk from her diet. However, fermented milk products are not prohibited. Nutrition for older children should be structured according to the same principle.

The ban on fermented milk products does not apply due to the fact that in them the protein is broken down into amino acids, which are much easier to digest by the children's digestive system. Babies with this disorder are allowed to introduce yogurt, fermented baked milk, and cottage cheese into their diet from approximately 6-7 months of age.
When choosing complementary feeding products, it is recommended to give preference to trusted brands that are marked “For children.”
Blend selection
Most companies producing adapted infant formula make their products based on cow's milk. This food is not suitable for children with allergies. Preference should be given to mixtures based on goat milk. Their list includes:
- FrisoPep AS.
- Nutrilon Pepti TSC.
- Nutricia Pepticate.
You might be interested in: Analogue of Primadofilus for children
They usually use a milk substitute. For babies with a hereditary predisposition to the inability to break down protein, it is recommended to buy mixtures such as NAN Hypoallergenic, Nutrilon Hypoallergenic, Humana, HiPP.
After 6 months, you can offer the baby the usual mixture, one teaspoon at a time. In the absence of negative symptoms, its volume can be gradually increased.
What to replace milk with?
Experts believe that if cow protein intolerance develops, you should not look for an alternative by offering your baby goat or sheep milk. It is especially not recommended to do this before the baby reaches two years of age. Of course, we cannot exclude the possibility that the child may develop an allergy solely to cow's milk. Parents should weigh the pros and cons before offering milk from other mammals to their child.
Allergy to milk in a child over one year old
When the immune and enzymatic systems are finally formed, this allergy goes away. While there is a rash or other manifestations of an allergic reaction, milk should be completely excluded from the child’s diet. If desired, milk of animal origin can be replaced with vegetable milk:
- Soy milk - obtained from soybeans. They are rich in protein and minerals. This milk can be obtained at home. You should soak the beans, then boil them and grind them to a puree, strain, and the milk is ready.
- Oat milk is a rich source of minerals and vitamins. Oats in husks are washed, poured with water and boiled over low heat for more than an hour, filtered and the finished product is obtained.
- Rice milk - to obtain it, you need to cook rice, grind the resulting porridge in a blender and filter.
Such a diet for milk allergies in children will help diversify their diet. Older children can also consume goat milk products.
Characteristic symptoms

Let's look at how a child's milk allergy manifests itself and the symptoms of this disease. Parents should know that the body’s response can be detected from the respiratory system, intestinal function and the appearance of characteristic signs on the baby’s skin. This is due to the fact that the allergen enters the bloodstream and spreads throughout the body.
- Respiratory system symptoms:
- allergic rhinitis;
- frequent sneezing;
- nasal congestion;
- cough;
- wheezing, wheezing.
It is important to know that if you experience a barking cough, loud wheezing and difficulty breathing, you should urgently call an ambulance. Such symptoms will indicate laryngospasm or the occurrence of pulmonary obstruction. If measures are not taken in time, the baby will begin to choke.
- Symptoms appearing on the skin:
- milk scab - this phenomenon has the form of a crust that is located on the head of a toddler, more often found in artificial babies;
- childhood eczema - observed on the child’s cheeks; first, bubbles with serous fluid appear, which subsequently disappear, forming erosions; As they heal, they become covered with crusts and dry scales. This symptom is most often observed in children under 6 months of age;
- urticaria - characterized by the presence of a small rash that causes severe itching and constantly itches; the skin becomes red and inflamed;
- atopic dermatitis - characterized by the appearance of red spots on the body, limbs and face of the child, severe itching is caused, which is why the child intensively scratches the areas of allergy, which can lead to a secondary infection (the introduction of pathogenic microorganisms from the child’s nails to the scratched area);
- Quincke's edema is a dangerous diagnosis that can even lead to death; characterized by severe swelling of the mucous membrane in the neck and face. During swelling of the larynx, asphyxia may begin and anaphylactic shock may develop.
- Manifestations from the gastrointestinal tract:
- nausea, vomiting;
- regurgitation in large quantities immediately after eating;
- intestinal colic, causing severe pain;
- diarrhea, pieces of undigested food and mucus are present;
- flatulence;
- reduction in weight gain.
Parents should know that if there are bloody streaks in the stool, as well as obvious symptoms of dehydration, the toddler must be urgently taken to the hospital.
An allergy to cow's milk in a child is manifested by restlessness, moodiness, crying, and abdominal pain. Attacks can be either short-term or permanent. As a rule, pain is observed in the navel area.
To visualize what a milk allergy looks like in a child, here are photos of these manifestations:

Childhood eczema
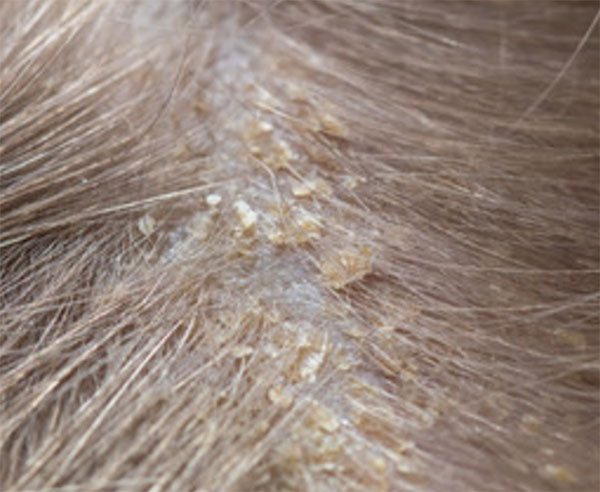
Milk scab

Atopic dermatitis
Forecast
There are more and more children with allergies in recent years. Nowadays diagnostics are much better developed than decades ago and it is much easier to determine what is causing the allergy. When the “enemy” is known, it is easier to fight it. According to various data, 40-50% of children cope with allergies by the end of the first year of life, 80-90% recover by 3-5 years, and in rare cases, allergies persist throughout their lives. In extreme cases, fermented milk products can completely replace the lack of milk in the diet.
Recently, American scientists conducted an interesting experiment. They studied the immune response in children with allergies who consumed more milk every day. And they found out that over time, skin manifestations decreased, and the immune system no longer reacted so strongly to the allergen.
They concluded that drinking milk would train the immune system and allergy symptoms would disappear in the future. So far, this point of view is not supported in our medicine; time will tell whether this is actually true.
Author:
Selezneva Valentina Anatolyevna physician-therapist
Nutritional Features
For children under one year old, it is difficult to find a complete milk substitute, because the baby gets everything he needs from milk. Both at a very early age and later, protein continues to be an important building material for the body, and the daily protein intake comes from dairy products. Therefore, it is so important to find the answer to the question: how to replace milk if a child has allergies.
The most difficult thing is to create a diet with a sufficient amount of all the necessary substances. To do this, use specialized vitamin-enriched baby food: fruit and vegetable purees, adapted baby milk, cereals, and meat purees.
After eliminating dairy products, the fat deficiency is corrected by increasing the dose of vegetable oil: from 5 to 10 ml for each meal. Protein deficiency is compensated by increasing the volume of meat products by 2-3 times.
Important! It is highly undesirable for children under one year of age to consume whole animal milk. Therefore, all dairy products are included in the diet in the form of special infant formula.
For artificial babies, formulas based on soy or goat's milk are selected, since an allergy to goat's milk occurs less frequently in a child. This is due to the smaller size of protein and fat particles in goat milk. Therefore, it is easier for the digestive system to absorb them.

The strict ban on milk does not apply to fermented milk products such as kefir, homemade yogurt, fermented baked milk and cottage cheese. In fermented milk products, when fermented, the protein breaks down into simpler and smaller compounds that are better absorbed by the body. However, such products must be introduced one at a time and then observed for the reaction.
Did you know? With properly selected nutrition, as they grow older, sensitivity to milk proteins disappears in 45% of children by the end of the first year of life, and in 80% improvement occurs by 4-5 years.