When preparing for childbirth, it is important for all expectant mothers to know what color newborns usually have, where it comes from, and why it is needed. The appearance of a dark sticky mass in a baby’s diaper is a good sign, which indicates that the baby’s intestines have begun to function properly.
Meconium in a newborn's diaper
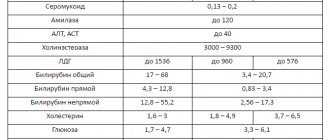
Norms of indicators of original feces
Meconium in newborns does not have any strong odor. The consistency of this mixture is viscous and sticky, resin-like. The color of the original feces in a newborn can be dark green or green-black, eggplant. The greenish or swampy tint of stool is due to the content of bilirubin, which is formed during the breakdown of red blood cells.
The average amount of stool reaches 60-100 grams. A newborn's feces are usually sterile and do not contain any germs.
Important! If a baby's poop is green in color and has a distinct putrefactive aroma, this may be a sign of dysbiosis or lactase deficiency.

Diaper with feces
Meconium aspiration syndrome
Mortality from aspiration of meconium by a baby during childbirth or in the prenatal period reaches more than 10% of all cases. The syndrome can occur even several days after birth. The syndrome of imaginary well-being is formed as a result of compensatory reactions of the baby’s body, which is accustomed to surviving in conditions of hypoxia throughout the entire period of pregnancy.
Symptoms
During aspiration of contaminated amniotic fluid, small particles of meconium penetrate into the opened alveoli and contribute to the disruption of alveolar oxygen exchange between the blood and lungs, as well as the destruction of surfactant. As a result, atelectasis of the lung area occurs - it is excluded from the respiratory act. The child shows signs of respiratory failure:
- breathing movements become more frequent and superficial;
- auxiliary muscles are connected to the act of breathing (the wings of the nose expand, the intercostal spaces retract, the supraclavicular fossae recede);
- breathing becomes noisy;
- the heartbeat increases compensatorily;
- the child is restless at first, then becomes lethargic, drowsy, and consciousness is depressed;
- the skin becomes cyanotic.
Be sure to read:
Stool color in newborns: where is the norm and where is the pathology?
When the doctor auscultates the child, moist rales of various sizes are heard, characteristic of the development of pneumonia, sometimes parts of the lung are not audible at all. The x-ray shows areas of triangular darkening (atelectasis) - collapse of the lung. Replacement emphysema is often observed around this area - an increase in the airiness of the lung tissue.
Complications
The provoked area of the lung is often overlaid with a secondary infection and the development of an inflammatory process. Since the newborn’s immune system is immature, and the baby is in a state of hypoxia, this condition can develop into a septic process.
In addition to the development of the infectious process, prolonged hypoxia contributes to the suppression of nervous tissue, including the death of areas of the cerebral cortex, which manifests itself in the form of hypoxic-ischemic encephalopathy. The child may subsequently lag behind in motor and psychological development, and the risk of developing cerebral palsy and epileptic syndrome increases.
Therapy
In this condition, the child needs treatment in intensive care in the intensive care unit:
- the child is connected to a ventilator, air is supplied under pressure, which allows the area of atelectasis to be mechanically straightened;
- Lung lavage is performed using repeated injections of saline and its immediate suction (this allows meconium particles to be removed from the affected areas);
- surfactant is introduced;
- Antibacterial therapy is prescribed to prevent septic conditions;
- feeding is carried out through a tube;
- Neurological drugs are introduced to help protect brain tissue from hypoxia (Actovegin, Ceraxon, Encephabol and others).
In continuation of the topic, be sure to read:
- Undigested food in a child’s stool: why does it appear and what does it mean?
- Pinworms in children: how do parasites manifest themselves and how to get rid of them?
- Giardiasis in a child: how is the infection manifested and treated?
- Ascariasis in children: how is helminthic infestation manifested and treated?
- Psychological constipation in a child 2-4 years old: methods of overcoming
- Yeast fungi were found in a child’s stool: is it dangerous and is treatment necessary?
- Gastroenteritis in children: how does the pathology manifest itself and be treated?
- Short bowel syndrome in a child: treatment and prognosis for life
- Celiac disease in children: how does the pathology manifest itself and be treated?
- Lactase deficiency: how is pathology manifested and treated in infants?
Be sure to read:
Hemocolitis in children: causes, symptoms and treatment (nutrition, medications)
When should meconium pass?
How long does it take for newborns to pass meconium? As a rule, four out of five babies pass their first stool 8-10 hours after birth or directly during the birth process. Within 2-3 days, the meconium completely leaves the baby’s intestines, and the baby begins to have transitional stool (it may contain particles of milk and meconium residues). At the age of one week, the baby's stool is completely normal.
Since original feces have a very viscous consistency, it is quite difficult to remove from the newborn’s body. In those children whose mother began breastfeeding immediately after birth, meconium passes much faster. This is due to the fact that colostrum released from the breast contains a sufficient amount of nutrients and has a mild laxative effect on the baby’s body.
Note! While in the mother's womb, meconium is excreted by about 10% of babies, the remaining 90% get rid of the original feces during the birth process or within 2-3 days after birth. Komarovsky states that passing meconium after 24 hours is normal.
Since meconium has a sticky and viscous consistency, it is not easy to wipe it off the baby’s skin - it will not be washed off with ordinary running water and soap. In order to wash it without extra effort and not cause harm to the baby, it is better to use special baby oil, gel or diaper cream. By dropping a few drops of the product onto a cotton pad, you can easily wipe off stuck poop from the butt and wash your baby in the shower. To avoid injuring the baby, do not rub the delicate skin too much.

The process of changing a diaper for a newborn baby
Meconium in the waters
(Translation: Ekaterina Zhitomirskaya-Shekhtman)
Green waters during childbirth.
Meconium itself is not a problem unless it is a symptom of severe fetal distress. And then the problem is in the condition of the fetus, and not in the appearance of meconium itself. If the fetal heart rate is good and labor is normal, even large amounts of meconium are rarely a problem.
Meconium is more common during induced labor, regardless of the method of stimulation, and the question of whether meconium passes more often during labor after the 40th week remains open, since such labor is also stimulated more often. I recently came across a study looking at whether intrauterine meconium passage actually poses a risk of meconium aspiration to the baby.
It is old, but large – almost a thousand births “with a large or medium amount of meconium” in the waters are considered.
Various factors have been identified that influence the amount of meconium; but only a few children out of every hundred actually demonstrated meconium aspiration syndrome (MAS), although all the children studied passed meconium in utero (MAS was found in 39 of 937 infants).
Stimulation is closely associated with both intrauterine meconium passage and meconium aspiration, but (and this came as a surprise to everyone), postmaturity was not a risk factor for the development of meconium aspiration syndrome: CAM was evenly distributed among women who gave birth at different stages.
Induction of labor was directly related to CAM.
We know that in babies born in induced labor, meconium in the waters is more common, and SAM is more common. It would be logical to assume that we more often encounter intrauterine meconium discharge during labor after the 40th week due to the fact that stimulation at this period is much more likely than at 40 weeks.
This study confirms what most of us have already seen: meconium itself is “rarely a problem.” Even if it's thick.
Why doesn't meconium pass?
If original feces (another name is meconium) do not leave the newborn’s intestines during the first day of life, this is considered delayed meconium passage. This situation can happen for some reasons.
Possible reasons
The most common reasons why meconium is delayed:
- Congenital pathology of the gastrointestinal tract, which leads to impaired patency;
- A disease called Hirschsprung syndrome. A congenital anomaly in which the intestinal nerve fibers responsible for regulating its motility are absent or underdeveloped. In this condition, obstruction of the affected area occurs. The intestinal sections become filled with foul-smelling feces and become greatly dilated;
- Underdevelopment of the function of the gastrointestinal tract. In this case, secretion and intestinal motility decrease, which causes blockage of the stool;
- Cystic fibrosis. This is a severe congenital disease that is inherited in an autosomal recessive manner. With this deviation, the pancreatic secretion acquires a viscous consistency. The organ begins to produce insufficient amounts of the necessary enzymes. Liquid absorption from the intestinal lumen begins to increase. With such an anomaly, the consistency and process of passing meconium change;
- Meconium plug syndrome. Occurs when original feces accumulate in the large intestine. This may occur due to impaired motor skills of this organ. Meconium plug syndrome most often occurs in babies born to mothers with hypermagnesemia or diabetes mellitus.
Meconium ileus
Meconium ileus is a congenital pathology in which obstruction and blockage of the large intestine occurs with original feces. In 15 out of 100 premature babies, such an anomaly occurs together with cystic fibrosis, a systemic disease that disrupts the proper functioning of the respiratory, reproductive, and digestive organs.
Additional Information. Meconium ileus begins to develop due to the lack of a pancreatic enzyme (trypsin). The lack of this hydrolase in the body provokes an increase in the viscosity of gastrointestinal secretions. Because of this, the stool becomes like caviar, sticks to the intestinal mucosa and cannot leave the rectum.
Symptoms
The main symptom of meconium ileus appears during the first two days of a newborn's life. You can suspect that something is wrong with the baby by the absence of stool within 1-2 days after birth. On the second or third day, the baby’s condition begins to deteriorate significantly. The child behaves very restlessly and constantly cries. He stops eating and cannot sleep properly. The baby begins to spit up frequently. In the vomit you can notice an admixture of feces and bile.
As the disease begins to progress, additional symptoms are added:
- The stomach becomes swollen and begins to hurt sharply;
- Skin turgor decreases;
- The skin turns pale;
- The child develops pronounced apathy;
- The baby becomes very inactive.
Then obvious signs of dehydration and intoxication begin to appear:
- Heartbeat accelerates;
- Blood pressure increases;
- The baby feels very thirsty;
- The dryness of the skin increases.
Intestinal obstruction is easy to identify by palpating the anterior wall of the abdomen - through the baby’s soft tummy you can clearly feel the blockage of feces. In this case, the child needs help as quickly as possible.

baby crying
Diagnostic methods
To confirm the diagnosis and identify the cause of the pathology, the doctor usually prescribes the following diagnostic methods:
- Plain radiograph of the abdomen. In the picture you can see distended intestinal loops. The presence of gases and solid meconium will appear as ground glass and soap bubbles.
- Irrigography. Gastrografin is injected into the rectum through an enema and an x-ray is taken. With meconium ileus, the large intestine will be empty, it will be very narrow, and filling abnormalities will be visible in the distal ileum - hard lumps of original feces. Using this study, you can easily determine the location of intestinal blockage.
- Computed tomography. With the help of such diagnostics, you can detect the causes of intestinal obstruction, conduct an X-ray examination from different angles, and then obtain a three-dimensional picture on a computer monitor.
- Ultrasound. After conducting such a study, you can see structural disorders in the abdominal organs, pseudocysts, and calcifications in the intestines.
- Sweat test. Using this test, you can determine the presence of chlorides in the secretion of the sweat glands. This is the most important laboratory test that helps diagnose cystic fibrosis. The test is performed on all newborns with meconium ileus.
Why is it dangerous for a child's life?
The most dangerous consequences of this condition are necrosis of all parts of the intestinal tract and inflammation of the abdominal cavity (peritonitis). Other extremely undesirable consequences include perforation of the colon, neoplasms in the form of pseudocysts, and very severe intoxication of the body with feces.
How to detect the presence of suspensions in amniotic fluid?
There are three main methods that allow you to study the state of amniotic fluid and its transparency:
- Ultrasound is the simplest and safest test for amniotic fluid, which allows you to detect suspensions in the amniotic fluid.
- Amnioscopy is a specialized device that is inserted into a woman’s cervix and allows us to study the state of amniotic fluid. Most often, this method is prescribed for post-term pregnancy to determine hypoxia (oxygen starvation of the fetus).
- Amniocentesis is a puncture of the amniotic sac performed through the abdominal wall of the mother. This test for amniotic fluid can only be performed in the second trimester of pregnancy. In addition to characterizing the suspensions, the resulting analysis contains a decoding of the chromosome set and allows us to determine the presence of possible pathologies of fetal development.
DETAILS: Examination with a gynecological speculum, correct preparation and examination procedure.
The presence of suspension in the amniotic fluid does not require specific treatment. Medicines can be prescribed only when hypoxia is diagnosed, in order to thin the blood and improve uteroplacental blood flow and oxygen exchange, as well as to prevent oxygen deficiency.
When oxygen deficiency is detected, it is very important to regularly monitor the condition of the fetus and, if necessary, carry out early delivery to avoid the death of the baby.
When to call a doctor
Problems with the passage of primary stool can occur during the first 1-2 days of a newborn’s life; they can be diagnosed in the maternity hospital during an examination of the baby by a pediatric neonatologist.
While in the maternity hospital, all mothers need to know in what cases they should urgently seek help from a doctor:
- The child started vomiting;
- The baby's body temperature increased;
- The baby does not have a bowel movement for more than 24 hours after birth;
- The baby cries for a long time and behaves restlessly;
- The newborn refuses to eat.

Crying baby
Normal stool transformation in children
It is worth considering the normal and abnormal stool of a newborn baby. 5-7 days after birth, when the original feces are completely expelled, the newborn’s stool becomes baby-like, acquires a yellowish color, a mushy consistency, and the baby’s feces may also have a sour smell.
Important! A sour smell of stool in a breastfeeding baby is normal if nothing bothers him and the stool has a normal consistency.
Normally, a newborn's stool can be all shades of yellow and brown. Even a slightly greenish tint will be normal due to the fact that the baby has elevated bilirubin levels. As soon as the correct functioning of the enzymes responsible for digestion is adjusted, everything will return to normal. Sometimes the stool may contain mixed lumps and streaks of undigested food.
A one-month-old baby's stool may be too watery, similar to diarrhea, or thick, like sour cream. You should only worry if black stool appears too liquid or too hard, contains streaks of blood and may smell bad.
A breastfed baby of 3 months may have very frequent stools, almost after every meal. Having bowel movements up to ten times a day - this may be called a variant of the norm.
As the baby grows, the frequency of bowel movements also changes, for example, if a two-month-old and a three-month-old baby pooped up to 10 times a day, then a 6-month-old baby’s bowel movements will decrease to 5-6 times a day, and by one year it will be 1-2 times a day. day.
Often mothers worry about why their newborn’s stool has an odor? Babies who eat formula are more likely to suffer from constipation or an upset stomach, and the smell of feces can be putrid and smelly.
Note! Deviations may appear due to diseases of the digestive organs or changes in the diet of a nursing mother. It is important for mom to know what she can eat.
If, some time after birth, meconium is detected in the newborn, this is a clear reason to rejoice, since the baby’s intestines are working correctly. If the original feces are not in a hurry to pass, you should consult a doctor. Timely recognized pathology will increase the chances of recovery.