What it is
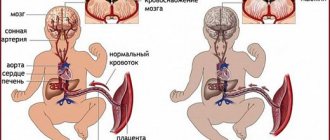
Normally, the heart ventricles are separated by a muscular barrier already at the time of birth. It not only makes up a third of their total area, but also takes an active part in every contraction and relaxation of the heart. The fetal organs receive only mixed blood. Both ventricles of the newborn are “busy with work” approximately equally, this explains the lack of difference in the thickness of their muscle walls.
Pathogenesis of circulatory disorders in VSD
The interventricular septum arises from three different structures, its formation is completed by 4-5 weeks of pregnancy. If fusion does not occur, a hole (defect) remains between the ventricles. It may be the only anomaly in the development of the heart (an isolated defect) or it may be combined with other congenital changes in the anatomy and be part of the structure of a combined defect. Today we are talking only about the first option.
In the first hours of your child’s life, after the baby begins to breathe, his entire blood flow system changes. The inclusion of the systemic and pulmonary circulation “forces” the baby’s heart to restructure its work:
- The pressure in the left ventricle increases significantly.
- With VSD, part of the blood enters not only the aorta, but also the right ventricle, creating additional stress for the latter. Experts call this process the discharge of blood “from left to right” (from the left half of the heart to the right).
- The right ventricle is “forced” to function more intensely in order to pump “extra” blood.
Changes in hemodynamics directly depend on the size and location of the defect. A small hole can close on its own (spontaneously) in a child by the age of 4-5 years. This usually happens in 65-75% of cases. With extensive defects, not only the right ventricle “suffers”. The pressure in the pulmonary circulation increases, and pulmonary hypertension occurs.
The baby’s body will try to compensate for the load:
- The mass of the ventricles increases.
- The walls of large and small arteries thicken.
- Thanks to these mechanisms, the pressure in both ventricles is equal. Despite the existing hole, blood discharge does not occur for some time.
- Gradually, the body's defenses are depleted, and the pressure in the right ventricle becomes greater than in the left.
- Venous blood will begin to flow through the defect into the systemic circulation - Eisenmenger syndrome. Decompensation of the defect occurs. Clinically, this process is manifested by the fact that the child begins to “turn blue.”
Fortunately, with early diagnosis and timely surgical treatment, this does not happen, even if the VSD is large. Therefore, try to listen to your doctor's advice. Of course, surgeons consider the best operation to be the one that the patient does not need to perform. But a ventricular septal defect in a newborn requires a thorough examination, specialist consultations, and a differentiated approach to patient management.
General information
Atrial septal defect (ASD) is one or more holes in the septum separating the left and right atrial cavities, the presence of which causes pathological discharge of blood, disruption of intracardiac and systemic hemodynamics. In cardiology, atrial septal defect occurs in 5-15% of people with congenital heart defects, while it is diagnosed 2 times more often in women.
Along with ventricular septal defects, coarctation of the aorta, and patent ductus arteriosus, atrial septal defect is one of the most common congenital heart defects. An atrial septal defect may be an isolated congenital heart defect or be associated with other intracardiac anomalies: ventricular septal defect, abnormal drainage of the pulmonary veins, mitral or tricuspid regurgitation.
Atrial septal defect
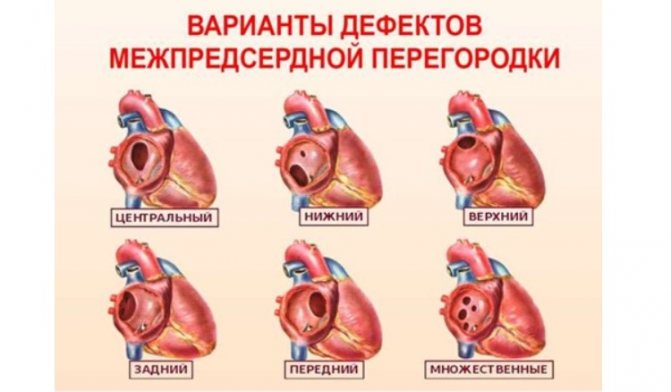
Classification of ventricular septal defects
According to the International Classification of Diseases, 10th revision (ICD-10), any VSD is coded with a code – Q 21.0. However, in practical pediatrics, doctors distinguish four anatomical types of this anomaly, according to the “Clinical Guidelines for the Management of Children with Congenital Heart Defects,” approved by the Association of Cardiovascular Surgeons in 2013:
- Subarterial ventricular septal defect. Located directly below the pulmonary valve. The aortic leaf can “bend” or “wedge” into the existing hole, which causes aortic regurgitation (reverse discharge of blood).
- Perimembranous ventricular septal defect - the hole is located in the membranous part adjacent to the tricuspid valve. The membranous septum can fuse with the defect, partially covering it.
- Inflow ventricular septal defect is localized in the inflow portion of the right ventricle.
- A muscular defect of the interventricular septum can be located in the center of the muscle, in the upper part, or at the border between the wall of the right ventricle and the septum itself. Sometimes several small holes are detected at once (multiple type of muscular VSD - Tolochinov-Roget disease).
So that you are not frightened by medical terms, and it becomes clear where exactly the hole in the interventricular septum is in your child, I will try to explain further. Anatomists divide this structure into three parts - upper (membranous), middle (muscular), lower (trabecular). Consequently, the trabecular defect is located in the lower part, the muscular defect is located in the middle part, and the membranous defect of the interventricular septum is located in the upper part.
Diagnostics
The main methods for diagnosing VSD include:

- Electrocardiogram . The study determines the degree of ventricular overload, as well as the presence and severity of pulmonary hypertension. In addition, in older patients, signs of arrhythmia and cardiac conduction disturbances may be detected.
- Phonocardiography . Using FCG, you can record high-frequency systolic murmur in the 3rd-4th intercostal space to the left of the sternum.
- Echocardiography . EchoCG allows you to identify a hole in the interventricular septum or suspect its presence based on circulatory disorders in the vessels.
- Ultrasonography . Ultrasound evaluates the work of the myocardium, its structure, condition and patency, as well as two very important indicators - pressure in the pulmonary artery and the amount of blood discharge.
- Radiography . On a chest x-ray, you can see an increase in the pulmonary pattern and pulsation of the roots of the lungs, a significant increase in the size of the heart.
- Probing of the right cavities of the heart . The study makes it possible to detect increased pressure in the pulmonary artery and ventricle, as well as increased oxygenation of venous blood.
- Pulse oximetry . The method determines the degree of oxygen saturation in the blood - low levels are a sign of serious problems with the cardiovascular system.
- Catheterization of the heart muscle . With its help, the doctor assesses the condition of the heart structures and determines the pressure in its chambers.
Differential diagnosis is carried out with aortopulmonary septal defect, pulmonary artery and aortic stenosis, mitral valve insufficiency, thromboembolism and other defects and diseases of the cardiovascular system.
Doctor's advice
Repeatedly, parents tormented themselves and me, trying to find out the exact etiology of the child’s congenital defect. When such a diagnosis is discovered in your own child, you definitely want to find the culprit. Grandmother on my father’s side sometimes blames my daughter-in-law for “bad genetics,” and my mother’s relatives blame her son-in-law for smoking and drinking alcohol.
I strongly advise you not to do this. Of course, it is important to find out the reason in order to predict the birth of healthy or sick children from the parents and the child himself. A baby with a VSD will someday become a father or mother himself. But a little person’s illness is not a reason to sort things out. Forget family quarrels. Focus on taking care of the baby.
ventricular septal defect | Women's magazine online - EVA.RU | Pregnancy
- Girls, today at 22 weeks I was diagnosed with an ultrasound - VSD (not clinical) up to 1.5 mm - in words the doctor said 1 mm. What to do about it? It will overgrow on its own and what should I eat and drink to make it overgrow? Will it increase as the fetus and heart grow? I'm sitting crying...
- You need a consultation with a good ultrasound specialist. Don’t cry just yet, sometimes uzists...at 20 weeks they can’t distinguish a pussy from a M, what can we say about a re-fencing and 1 mm.
- We went through this... Only the diagnosis was made after giving birth. Your baby’s defect is small, most likely it will close on its own (if it is located in the muscle layer) as the heart muscle grows. We had no restrictions, the defects (there were 2 of them) completely closed by the age of 6. As I understand from cardiologists, this defect is considered the most favorable in terms of self-healing. Don't cry, take care of your nerves. Everything will be fine.
- There was also a VSD, I can’t say what size. And there was also the defect Tetralogy of Fallot. Interrupted….
- it was Tyo(((he said not to worry yet, maybe it will go away on its own... And if it doesn’t go away? Why does the baby have such crap? If only from the Moscow smog...
- We were diagnosed with premembranous – where is it? thanks for support…((
- I read about Fallot, it’s absolutely terrible. Sorry…
- go to Stygar/Demidov/voevodin
- We were also diagnosed with a VSD. They did an ultrasound in several places, and, for example, in the Center for Surgery and Rectification a defect of up to 2 mm is not noted at all in the features, in 29 r/d too. At 20 RD, where I was in the hospital, this VSD was not noticed at all. We went to do an ultrasound at the perinatal center at Bakulevka. Our slit-like gap was 1.8 mm at 30 weeks, the prognosis was favorable: it should heal before birth or before the child’s 1st year. They told me not to be nervous and to come for a follow-up ultrasound at the baby’s 1st month. Author, I advise you not to worry yourself and your child’s nerves once again. And to reassure you, if you really want it, then it’s better to do an ultrasound in Bakulevka so that they can look at it in profile.
- thanks for the answer! I’ll probably go to Bakulevka, when is the best time to do this - probably at the next scheduled ultrasound, at 30 weeks? or go right now? Please write when you were diagnosed with this and what the dynamics are - does the defect increase as pregnancy progresses or vice versa?
- It should be overgrown. At 31 weeks I was diagnosed with a 2 mm VSD (plus a bunch of heart problems), then I was observed in Bakulevka. So, up to 2 mm VSD are not considered serious defects at all. After birth (on the 7th day), we did an echocardiogram of the baby - the VSD was already 1 mm, and our other problems were also much smaller - everything heals over time, because... As the child grows and the heart enlarges, such things usually take longer. You have a chance that the VSD will heal by the time you give birth. If you want, write to me in a personal message - I’ll tell you in detail about Bakulevka and others.
- Same story as yours. Cho made the same diagnosis, the same dimensions. The doctor sent me to Bakulevka for an ultrasound at 28-29 weeks. In general, she reassured me and said that the prognosis was favorable. I’ll go there at the end of October.
- He also scared me by saying that many heart defects cannot be diagnosed by prenatal ultrasound (what if there is something else there(
- They gave it to us. In fact, the birth of the VSD was not found!
- He tried to calm us down, saying that after birth we definitely need to do an ultrasound of the heart, and then everything will be clear. And so, he expressed the hope that the defect would heal by birth. After 4 weeks I had a scheduled ultrasound (not in Bakulevka, I’ll just go there), but the doctor didn’t say anything and didn’t see anything.
- What was the size of the defect when the diagnosis was made?
- My son was born with a VSD of 2.8 in the muscular part, at 7 months the defect began to close, after a year we’ll go and see. It’s important in which part, in the membrane part it’s bad, it won’t close, in the muscle part it’s better, most likely it will close, what’s important for well-being is the amount of blood discharge, the less the better. Often a small VSD in the muscular part is called “much ado about nothing.”
- There is a muscular layer, which is closer to the apex of the heart, and there is a membranous layer, closer to the atria and valves. We had one in the muscle layer (it closed earlier), the other was closer to the membrane, closed later, but also nothing criminal. And the size was larger than yours. All our worries are due to lack of information, I cried so much in the maternity hospital, they didn’t know what to give me. And then all the doctors explained everything in detail and immediately I felt calmer. Believe me, our children do not have the most serious health problems.
- This happened with us, but I didn’t know about it before giving birth (and it’s bad that I didn’t know). I advise you to go to the maternity ward at Bakulevo) After birth, watch the child there and it happens that the defect does not diverge (this depends on the location of the defect on the septum) If it starts to diverge, then surgery. Yes, it’s not easy, but it’s not fatal (7 days in the hospital and you’re home). My daughter is already 5 years old (the operation was done when she was one year old) and is a normal, cheerful child. Yes, she doesn’t really like active games (apparently the body insures itself), but so what, but she draws well. Don’t cry, this is bad for the child, the child must feel support from you and be calm, otherwise he will not pass the test. GOOD LUCK!
- Can I ask a question - tell me, did this defect manifest itself in any way externally? Were there any symptoms in the first year of life - blueness around the mouth, cold hands, sweaty feet? How did you find out about the defect?
- This was not the only heart defect we had (but I learned this when the baby was 4 months old). Her hands were cold (but they were cold by definition), and there was no shortness of breath, no sweating when sucking. For us, defek gave an unpleasant sound when breathing (you know, like when you have bronchitis, there is wheezing). That’s what happened to us. That's why they started to investigate. But I didn’t immediately realize about Bakulevka, so the operation took a year, but it would have been better in 4-6 months. It’s just that children begin to walk when they are one year old and it is very difficult to restrict them from doing so, even for a week.
- Why go to them if they don’t specialize in the heart? Moreover, the author clearly does not have a gross defect in the baby! Well, Voevodin wrote to me at 25-26 weeks with a suspicion of VSD, so what? In Bakulevka they at least gave me some kind of forecast and explained everything. By the way, when I was in Bakulevka, the doctor told me that recently it was from the recognized luminaries Stygar/Demidov/Voevodin (“the old guard”) that recently a lot of pregnant women come for examination, and sometimes they are overly frightened to the point of abortion, Moreover, defects or developmental anomalies in the fetus are completely curable in practice. Voevodin also gave us only a 5% positive outcome, but we believe that everything will be fine for our baby!
- Is it possible to get to Bakulevka for an ultrasound without a referral?
- This is the only way you can do it, no directions are needed, everything is paid
- Thank you very much everyone for your support, I calmed down and decided not to freak out ahead of time. I asked a question on the forum of the Bakulevka perinatal center - they answered that the probability of closure is high and it is necessary to do a careful ultrasound at approximately 32 weeks. In general, I walk, eat fruits and vegetables and pray to God that everything will go away on its own.
- We were diagnosed with a VSD at 13 weeks, 1.3mm, referred to a pediatric cardiac surgeon for an ultrasound, he had a VSD at 22 weeks, he diagnosed a VSD in the muscle 1, 2mm and 1mm, but said that there was no need to worry, it should be overgrown in utero and gave a referral for an ultrasound at 30 We'll see how the baby and the heart behave in a few weeks
Source: https://eva.ru/pregnancy/messages-2422762.htm
How to suspect a defect: symptoms and signs in a child
If the hole size is small, your baby will be no different from his peers. Probably, even in the maternity ward, the neonatologist will report that your baby has a systolic heart murmur. Parents usually ask with alarm at each auscultation: “Has the noise decreased or become stronger?” The paradox of VSD is that the intensity of the noise is inversely proportional to the size of the hole. The weaker the noise, the larger the size of the defect.
The situation is more serious if the baby was born “without noise”, but:
- from three to four weeks of age, he suddenly stopped gaining weight when the mother had enough milk;
- he developed shortness of breath during feeding;
- respiratory infections “pursue” him more often than other children;
- sometimes the child begins to “turn blue”;
- upon examination, the doctor suddenly discovers an expansion of the borders of the heart and an enlargement of the liver.
Subsequently, the clinical picture is characterized by a diffuse, intensified apical impulse, the appearance of systolic tremors on the left in the third and fourth intercostal spaces, expansion of the borders of the heart, especially to the left, and the formation of a cardiac hump (Davis chest).
Diagnostic methods
Auscultatory data and other symptoms will allow the pediatrician to suspect a congenital malformation in the child. Most likely, to clarify the diagnosis, the pediatric cardiologist will write a referral to:
- X-ray of the chest organs - if the defect is small, no changes will be detected. If the hole is of a significant size, hypertrophy of the left atrium and ventricle and an increase in the pattern of the lungs may be detected. In case of complication of VSD with pulmonary hypertension, bulging of the pulmonary artery arch with a weakening of the lung pattern and a non-hypertrophied left ventricle.
- Electrocardiography - in the differentiation of heart disease is not of particular importance, but will reveal a deviation of the electrical axis, as well as signs of overload of both or only the left ventricle.
- Echocardiography is considered the main diagnostic technology for heart defects. The ultrasound examination method makes it possible to clarify the exact location of the hole, its size, the number of defects, and also evaluate changes in hemodynamics. The main purpose of ultrasound is to directly visualize the defect and exclude other cardiac anomalies. Doppler mapping will help determine the magnitude of the discharge, the presence of blood regurgitation, and assess the systolic pressure in the right ventricle.
If the defects are not clearly visible on echocardiography, or the doctor suspects a combined heart defect, you may need to undergo magnetic resonance or computed tomography.
Cardiac catheterization and angiography
Typically, these diagnostic techniques are rarely prescribed to children, but if non-invasive methods do not provide complete information about the condition, they are performed to assess hemodynamics in the pulmonary circulation and pulmonary hypertension. During this procedure, pressure in the aorta and pulmonary artery is measured, and the gas composition of the blood inside the heart chambers and large vessels is determined. Conducted by experienced specialists in regional centers.
Diagnostic methods
Methods for diagnosing VSD:
- Anamnesis collection. Questioning parents about hereditary diseases, the presence of heart pathologies in relatives, the course of pregnancy, medications taken in the first trimester and past illnesses, etc.
- Medical examination. It consists of measuring the pulse, auscultation of the heart (listening to murmurs), examining the color of the skin and changes in the shape of the chest, palpation in the heart area. With VSD, this method in most cases already makes it possible to make a diagnosis.
- Echocardiography. The defect is displayed as a rupture of the echo signal in the interventricular septum with a reset detected in continuous wave and color Doppler modes.
- MRI. It is carried out when there is insufficient information from echocardiography or the result is unclear.
- Catheterization of cardiac cavities. Allows you to check the hemodynamics of the pulmonary circulation, the number, size and location of defects, and the presence of associated anomalies.
- Radiography. Used to diagnose large VSDs and pulmonary hypertension. Small defects are not displayed.
- ECG. Both small and large defects are diagnosed by axis deviation.
- Laboratory diagnostics. A complete blood count is taken to determine hemoglobin levels. Done if surgery is necessary.
Although the presence of a defect is revealed by listening to the heart, the child should be shown to a cardiologist if his skin turns blue or his legs swell. In most cases, the diagnosis becomes known after examination.
Electrocardiogram
If necessary, a study is carried out to determine the increase in load on the right ventricle and the increase in pressure in the systemic circle. An electrocardiogram helps identify signs of changes in a child's heart rhythm.
Phonocardiography
Using a special device, it is possible to record high-frequency noises arising in the heart.
Echocardiography
A technique based on the reflection of an ultrasonic signal helps to identify changes in blood circulation in large vessels and detect a hole in the septum.
To find out whether the pressure in the pulmonary artery has increased, scan the heart muscle, check the patency of the myocardium, and determine the level of blood discharge, perform an ultrasound.
Radiography
When examining the chest, radiation passing through the baby’s body displays a picture on the screen that allows one to evaluate the pulsation of the roots in the lungs and examine the heart.
When using this diagnostic method, the pressure in the pulmonary artery and the change in the load on the ventricles are determined, which indicates the presence of a problem in the organ cavity.
Pulse oximetry
The test is carried out to find out whether there is enough oxygen in the blood. With severe myocardial pathologies and vascular diseases, the saturation indicator drops.
To check the condition of the parts of the organ and measure the pressure in the chambers, a manipulation is performed in which a flexible tube is inserted into the organ through a vessel in the groin and on the arm.
Treatment of ventricular septal defect
The approach to the management of patients with VSD is strictly individual, depending on the size and location of the defect, clinical presentation (the occurrence of pulmonary hypertension, the development of circulatory failure), and the presence of concomitant pathology.
If the hole is small, there are no hemodynamic disturbances, the child only needs regular examinations by a cardiologist and periodic echocardiography. If there is the slightest doubt about the favorable course of the disease, surgical treatment is indicated.
There are the following types of surgical correction of VSD:
- An operation under artificial circulation, during which the cardiac surgeon sutures the hole or closes it with a valve.
- “Auxiliary” narrowing of the pulmonary artery is a preliminary surgical preparatory operation to prevent decompensation of the defect. Allows you to “buy time” before radical correction.
- Minimally invasive endovascular intervention. It is carried out under ultrasound and fluoroscopy control. Through the femoral artery, the vascular surgeon inserts a special device (spiral or occluder), passing it into the cavity of the heart, closing the defect.
- Hybrid operation. After opening the chest, an occluder is inserted directly through the myocardial puncture. The intervention protocol does not include stopping the heart and connecting it to the artificial circulation system.
A specialist decides which method is most suitable for your child. Without the written consent of the parents for surgical intervention, no doctor will operate on the child. It is important to discuss the progress of the operation with your doctor, choosing the most optimal tactics.
It should be remembered that if you miss precious time and do not close the hole before pulmonary hypertension develops, there is a risk of death from circulatory failure. Drug therapy is prescribed as preparation for surgery, during the rehabilitation period, as well as during the development of decompensation of the defect in order to support the functioning of the heart.
Treatment
Small septal defects that do not produce pronounced symptoms usually do not require any special treatment, as they heal on their own by 1-4 years of age or later .

In preparation for surgery, conservative treatment is used to help regulate heart rate, normalize blood pressure and support myocardial function.
Surgical correction of VSD can be palliative or radical : palliative operations are performed on infants with severe malnutrition and multiple complications in order to prepare for radical intervention. In this case, the doctor creates an artificial pulmonary artery stenosis, which significantly alleviates the patient’s condition.
Radical surgeries used to treat VSD include:
- suturing pathogenic holes with U-shaped sutures;
- plastic surgery of defects using patches made of synthetic or biological tissue, performed under ultrasound control;
- Open heart surgery is effective for combined defects (for example, tetralogy of Fallot) or large holes that cannot be closed with a single patch.
The best results are obtained from surgical interventions performed at the age of 2-2.5 years, when patients usually show the first signs of heart failure.
This video talks about one of the most effective operations against VSD:
Case from practice
In the maternity ward, the neonatologist suspected congenital heart disease.
Ultrasound examination revealed a muscular defect of the interventricular septum in a newborn. Cardiocenter specialists recommended surgical correction before the age of 6 months, since the size of the hole was too large. The parents were determined to undergo surgical treatment, but according to their faith, the pastor's blessing was required. And he, seeing a seemingly healthy girl, advised to postpone the operation a little. Like, she’s still very little, the vice doesn’t bother her, you’ll always have time to “cut” it.
At the seventh month of life, the baby showed the first signs of pulmonary hypertension, which we tried unsuccessfully to combat by prescribing medications. On the ninth - the parents begged the heart surgeons to save the child, but it was too late to operate - a heart failure clinic developed. The girl died when she was one year old.
And yesterday a young man came to the reception. Eighteen years. He was indignant that the draft board doctors sent him to the hospital for additional examination. He is involved in athletics. He dreams of entering a military school. I open the outpatient card, and there is surgical treatment for VSD. On the chest there is a thin strip of postoperative scar, almost invisible. The guy doesn't remember the operation. He sincerely does not understand what is wrong with him. It’s just that his parents weren’t afraid to “cut” him at one time.
Possible complications
Among the consequences:
- Pulmonary hypertension. Stable increase in pressure in the vessels of the pulmonary circulation. It affects health in several ways. Insufficient saturation of liquid tissue with O2, weak release of CO2, disturbances in cellular respiration. As it progresses, the so-called cor pulmonale develops. This is an irreversible defect that poses a risk to life.
- Heart attack. As a result of catastrophic ischemia (malnutrition) of the myocardium. Occurs mainly in the later stages of the condition.
- Stroke. Acute necrosis of brain tissue and cerebral structures. The likelihood of death is significant, but the chances of developing neurological deficits, from muteness to blindness and paralysis, are even higher.
- Children have insufficient physical and mental development, retardation. It is noticeable almost immediately and does not present any difficulties in diagnosis.
Despite all that has been said, the likelihood of such violations is relatively small. Usually doctors identify a defect before it has time to “make trouble” in the human body. The examination requires only tissue visualization. Next, there is the opportunity to decide on treatment.
Ventricular septal defect in a newborn and an adult has identical features both in terms of clinical manifestations and in terms of diagnosis and treatment.
The disorder is always congenital; correction provides a good chance of complete success. You can count on recovery and quality of life after treatment. If required.
Is it possible to diagnose a defect before the birth of a child?
Yes, you can. To do this, it is necessary to undergo a timely ultrasound examination during pregnancy by an experienced specialist using modern equipment. If your unborn baby is suspected of having a VSD, try to choose a maternity hospital closer to the cardiac center.
We often hear reproaches from parents that they followed all the doctors’ recommendations, but the heart defect was discovered only after the birth of the child. Unfortunately, a hole in the interventricular septum with a diameter of up to 4 mm is very difficult to detect without color Doppler mapping. Therefore, if you have a family history, smoked before pregnancy, or had the flu or acute respiratory viral infection when you were expecting a baby, be sure to tell your gynecologist about this. You may need to undergo additional ultrasound using more sensitive equipment.
Essence and mechanism
VSD in the fetus is formed in the first weeks of intrauterine development. Vice is not acquired. It is always innate.
Why this happens is not known exactly. It is assumed that negative influences on the mother during pregnancy are to blame. There are a lot of factors: from increased background radiation and poor nutrition to stress, alcohol consumption, and smoking.
In some cases, the defect is based on genetic factors.
It is known that children with Down syndrome and other chromosomal disorders, almost without exception, are born with a defect of the interventricular septum.
However, according to statistics, 96-98% of patients with diagnosed anatomical disorders do not have problems with genetics.
Since the exact mechanism has not been established, it is impossible to develop clear preventive measures to prevent the development of pathology. But she is being treated well.