Lymphadenitis in children is inflammation of the lymph nodes.
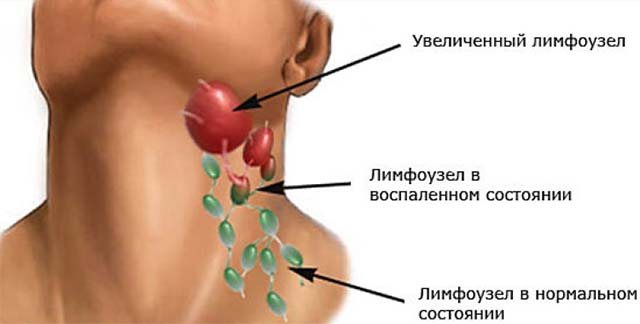
Lymph nodes are peripheral lymphoid organs, which are round anatomical formations of connective tissue filled with lymph. Lymph nodes are connected to the circulatory system by lymphatic vessels and postcapillary venules. As the lymph passes through the lymph nodes, it collects into lymphatic ducts, which open into the venous circulatory system. At the same time, the lymph nodes perform the function of biological and mechanical purification of the blood: they retain and accumulate antibodies, which form an important part of the immune system. At the same time, the lymph nodes play the role of a filter, inactivating bacterial agents present in the lymph. When foreign particles and bacteria, passing through a lymph node, become trapped in its trabeculae and septa, inflammation can develop. In the presence of a focus of inflammation, the lymph nodes become compacted and painful, increase in size, and lymphadenitis develops. Thus, lymphadenitis is not an independent disease, but a symptom of the main pathological process occurring in the body, a signal of a decrease in its protective functions.
Since the development of lymphadenitis is caused by a primary disease, the main measure to prevent inflammation of the lymph nodes is timely diagnosis and treatment of the primary pathology.
In children, lymph nodes have an incomplete structure; septa and trabeculae are not fully formed at an early age, which reduces their barrier function. The maturation of lymph nodes occurs gradually, by the age of 8-9 years an immunological response appears, and at 12-14 years the formation of lymph nodes is completed.
Causes of lymphadenitis in children
The most common cause of lymphadenitis in children is infectious inflammation caused by the following pathogens:
- staphylococcus;
- streptococcus;
- Pneumococcus;
- coli;
- Mycobacterium tuberculosis;
- Pseudomonas aeruginosa;
- parasitic and fungal infections;
- Epstein–Barr virus;
- AIDS virus.
Lymphadenitis in children is often associated with an inflammatory process in the oropharynx and nasopharynx with sore throat, flu, otitis media, adenoiditis, and chronic tonsillitis. Lymph nodes become enlarged during childhood infections - scarlet fever, rubella, mumps, diphtheria, as well as skin diseases - pyoderma, exudative diathesis, infected eczema. Penetration of microbes into the body can occur through the flow of lymph, blood, or through direct contact.
Non-infectious causes of lymphadenitis in children: lymphoma, secondary (metastatic) cancer of the lymph nodes, contact infection when infected material comes into contact with the tissue of the lymph node.
Why are the lymph nodes swollen and palpable?
Lymph nodes are organs that act as natural filters. They cleanse the lymph and help protect the body. When an infection enters the body, the lymph nodes begin to intensively produce lymphocytes - blood cells whose purpose is to fight for human health. This is the answer to the question why they sometimes become inflamed. To avoid this unpleasant moment, you should be attentive to the child’s health.
One of the causes of inflammation of the lymph nodes is oral infections. To avoid problems, you need to regularly brush your teeth and disinfect them on time, rinse your mouth with special products after eating. The cause of inflammation of the lymph nodes in the neck is infectious diseases. Any infection that enters one of the organs located in close proximity to the neck will cause swelling of the cervical lymph nodes.
On the one side
The causes of inflammation of the lymph nodes in a child’s neck are no different from the general causes of their inflammation. There are some features of unilateral lymphadenitis. If the lymph node in a child’s neck on one side is inflamed, tumor diseases can be suspected.

Unilateral lymphadenitis is caused by:
- dental diseases;
- upper respiratory tract infections;
- oncological diseases;
- pathologies of the thyroid gland;
- infectious diseases;
- HIV;
- immune system diseases;
- damage by microorganisms introduced after insect bites;
- purulent wounds.
Inflammation of the cervical lymph node on the left is a sign of infection in the mouth.
At both sides
Inflammation of the lymph nodes in the neck on both sides indicates damage to the entire body. Chronic infections lead to bilateral lymphadenitis: tonsillitis, tonsillitis, pharyngitis and others. The cause may be a lack of vitamins. If a child takes school very seriously, then constant tension and severe fatigue can lead to bilateral lymphadenitis. Quite rare, but there are still cases when enlarged lymph nodes in the neck on both sides signaled a metabolic disorder.
If the lymph node is enlarged only on the right, tuberculosis can be suspected. Lymphadenitis affecting the lower neck area is an indicator of infection of organs located below the neck. These lymph nodes collect lymph from the thoracic and abdominal areas. Disease of any organ in one of these areas leads to inflammation of the lymph nodes in the lower part of the neck. Sometimes this is a sign of breast cancer.
Behind
If a child has an inflamed lymph node in the back of the neck, it makes sense to visit an infectious disease specialist. This indicator can be a sign of rubella, which may go unnoticed.

The inflammatory process in the lymph node in the back of the neck is characteristic of post-traumatic conditions. If you have received injuries to the head or neck, arms, chest, or upper back, they may subsequently become inflamed, which will affect the lymphatic system.
If many cervical lymph nodes are enlarged
If many lymph nodes in the neck are inflamed, they are swollen and painful, then this process should be considered from the point of view of the baby’s age. In babies under one year old, pathological growth of teeth can cause pain in all cervical lymph nodes. This process occurs differently for all children. Some people's teeth grow slowly, appearing one at a time or in pairs. And for some, the process is going on rapidly.
Even if the teeth grow normally, the baby feels discomfort: the temperature rises and appetite decreases. And if the digestive organs decide to appear all at once, this will lead to severe inflammation of the gums and problems in several lymph nodes.
We recommend additional reading: What to do if your child’s ear is red, hot, sore or swollen
In older children, an increase in the series of cervical lymph nodes is associated with cytomegalovirus. This infection is a type of herpes. Like any herpes, CMV enters the body during life. It affects the digestive organs and respiratory tract. Once it enters the body, it remains there for life. It is impossible to completely get rid of it, but it can be blocked.
A strong immune system is the best assistant in the fight against any virus. It suppresses the infection and prevents it from developing.
Inflammation of several cervical lymph nodes may be a consequence of frequent colds. If a baby systematically catches a cold and suffers from acute respiratory viral infections, then sooner or later, this will lead to cervical lymphadenitis.
Types of lymphadenitis in children
Lymphadenitis is classified according to several criteria.
According to the etiological factor, they are distinguished:
- specific lymphadenitis - develops under the influence of pathogens of tuberculosis, syphilis, brucellosis, toxoplasmosis, actinomycosis, tularemia;
- nonspecific lymphadenitis - caused by pyogenic microbes (staphylococci, streptococci), their toxins, opportunistic bacteria, tissue decay products from the primary foci of the purulent process, fungal microorganisms living on the surface of the skin and mucous membranes.
Clinical manifestations of lymphadenitis are layered with manifestations of inflammation in the main focus, pain occurs in the corresponding areas.
Based on the nature and duration of the infectious process, lymphadenitis is distinguished:
- acute – characterized by a short prodromal period, occurs after wound infection, surgery, or when virulent microbial flora enters the tissue; clinical symptoms are pronounced;
- chronic - often the result of exposure to a weakly virulent infection during protracted, sluggish inflammatory diseases, progression of cancer, and an unfavorable outcome of acute lymphadenitis. It has a wave-like course, periods of exacerbation are replaced by remission.
Acute lymphadenitis, in turn, can occur in two forms:
- serous - occurs under the influence of viruses and tumors, usually accompanied by vague symptoms, inflammatory phenomena do not extend beyond the capsule of the lymph node;
- purulent - develops under the influence of a chronic bacterial infection, inflammation can spread to surrounding tissues, and poses a threat of developing sepsis.
Separate variants include hemorrhagic and fibrinous lymphadenitis.
The inflammatory process can affect one or more neighboring lymph nodes. According to the localization of the inflammatory process, lymphadenitis can be local, regional and generalized.
Symptoms of lymphadenitis in children
Symptoms of lymphadenitis in children:
- increased body temperature;
- leukocytosis;
- swelling in the area of the affected lymph node, enlargement of the lymph node;
- hyperemia with a local increase in temperature (with a superficial location of the inflamed lymph node).
The severity of symptoms is determined by the nature of the underlying inflammatory process and the type of disease.
The success of treatment of lymphadenitis in children depends on the timely detection of the disease and the adequacy of therapy.
Acute lymphadenitis in children is manifested by enlargement and local pain of the lymph nodes upon palpation, fever, weakness, and headache. Lymph nodes are mobile, but their boundaries lose their outline and merge with the surrounding tissues. Clinical manifestations of lymphadenitis are layered with manifestations of inflammation in the main focus, pain occurs in the corresponding areas (for example, the cervical lymph nodes become inflamed with sore throat, which is accompanied by a sore throat).
With serous lymphadenitis, the health of the sick child may not change. There is an increase and hardening of the regional lymph nodes, moderate pain, and no inflammation on the skin. Swelling of the tissues adjacent to the node may be observed.
The development of purulent destruction is indicated by sharp pain, fever, chills, weakness, loss of sleep and appetite. There is pronounced hyperemia of the outer integument over the superficially located node. The lymph nodes become immobile and fuse with each other and with adjacent tissues. In the absence of proper treatment, purulent inflammation spreads to the surrounding tissues, areas of softening appear, the boundaries of edema are blurred, diffuse hyperemia is determined, and a lymph node abscess or adenophlegmon may develop. This is accompanied by a sharp rise in temperature, the appearance of chills, tachycardia, intense headaches, and severe weakness.
Chronic inflammation of the lymph nodes is characterized by the absence of pain or its mild severity. The main symptom of chronic nonspecific lymphadenitis in children is enlargement of the lymph nodes, and they are usually dense to the touch, not fused to each other and separated from the surrounding tissues.
Lymphadenitis is not an independent disease, but a symptom of the main pathological process occurring in the body, a signal of a decrease in its protective functions.
In childhood, the period of primary tuberculosis is often combined with damage to the intrathoracic lymph nodes. Several groups may be involved in the process at once. A distinctive feature of tuberculous lymphadenitis is the presence of periadenitis (a conglomerate of affected lymph nodes fused together). With the acute onset of tuberculous lymphadenitis, there are symptoms of tuberculous intoxication, high temperature, enlarged lymph nodes, sometimes with pronounced inflammatory-necrotic changes.
About prevention
Despite the fact that lymphadenitis in the neck in childhood occurs faster than in adults, it is better treatable even at the purulent stage. However, if preventive measures are taken, the development of the disease can be prevented. Remember! The disorder often appears as a secondary inflammatory process against the background of another primary diagnosis.
Measures to prevent the disease are aimed at:
- increasing the body’s own strength and stabilizing the immune system;
- relief and complete elimination of possible chronic infections;
- timely dental treatment and frequent sanitation of the oral cavity.
With proper treatment of cervical lymphadenitis in children, positive results can be quickly achieved, especially at the serous stage. The main task of any parent is to consult a doctor at the slightest sign of the appearance of a focus of the inflammatory process. Delay and self-medication can be hazardous to health.

Psychosomatic causes of inflammation of the lymph nodes
Previous post

Features of T-cell lymphoma
Next entry
Discussion: 2 comments
- Asya:
01/10/2019 at 13:08My child recently encountered cervical lymphadenitis. One side of the neck seemed visually larger to me than the other. I touched the lymph nodes - and they were hard and enlarged. It hurt my daughter a little when I touched them. I first took her to the pediatrician, who examined her and prescribed a general blood test to rule out mononucleosis, from there I took her to a pediatric surgeon, who prescribed compresses with Dimexide for 10 days. She did not have a temperature, so she was not prescribed antibiotics. In the analysis, thank God, everything was clear, the compresses helped, but all this developed, as it turned out, due to tonsillitis.
Answer
- Maria:
01/11/2019 at 05:42
I encountered cervical lymphadenitis in my daughter and realized that most doctors have no idea how to treat this disease. The ENT specialist sent us to the dentist, citing the fact that the lymph nodes were inflamed due to the replacement of milk teeth with molars. Dentist - back to the ENT specialist and pediatrician. Having found a knowledgeable doctor, we took a course of antibiotics as prescribed, and then immunostimulants and vitamin complexes, everything went away.
Answer
Diagnostics
At the first stage of diagnosis, a physical examination of the child is carried out, an assessment of the clinical picture, anamnesis collection, and palpation of the lymph nodes. During palpation, the location, size, shape, cohesion, consistency, pain and mobility of the lymph nodes are noted. The examination of lymph nodes is carried out with both hands, in symmetrical areas, in comparison.

The examination plan includes:
- peripheral blood test - increased level of leukocytes (characteristic of diseases of bacterial etiology), predominance of lymphomonocytes in the blood count (indicates in favor of herpetic and other viral etiology);
- microbiological study of microflora from the oropharynx;
- a complex of serological blood tests using ELISA and PCR;
- allergy tests;
- HIV test;
- ultrasound examination of lymph nodes;
- X-ray examination;
- puncture biopsy of the lymph node.
Based on the results of the main examination, additional laboratory and instrumental studies may be prescribed to diagnose the primary disease.
In children, lymph nodes have an incomplete structure; septa and trabeculae are not fully formed at an early age, which reduces their barrier function.
Treatment of lymphadenitis in children
Treatment of lymphadenitis in children is aimed at eliminating the primary focus and stopping the inflammatory process in the lymph nodes. If the cause of lymphadenitis is a bacterial infection, then antibiotic therapy is prescribed using macrolides, aminopenicillins, cephalosporins, macrolides, and semisynthetic penicillins. The treatment regimen depends on the type of infectious agent and the characteristics of the child (weight, age). According to indications, desensitizing and restorative agents are prescribed, and symptomatic (painkiller and anti-inflammatory) therapy is carried out.
During the recovery period after acute lymphadenitis and in the process of treating chronic lymphadenitis, physiotherapeutic procedures are used (UHF therapy, laser therapy, quartz irradiation, galvanization).
In case of purulent melting of the lymph node, surgical intervention is indicated, which consists of opening purulent phlegmons and abscesses, removing their contents, treating the cavity with an antiseptic and establishing wound drainage. In the postoperative period, antibiotic therapy is carried out.
If tuberculosis is confirmed, treatment is carried out in a specialized (phthisiatric) department of the hospital.
Treatment

Therapy is applicable only after an accurate diagnosis and establishment of the causes of the disease.
The following medications may be prescribed to your baby:
- Etiotropic drugs in case of infectious nature of the disease. The course of treatment will consist of taking macrolides, cephalosparins, and immunomodulatory drugs.
- If the disease is of viral etiology, antiviral agents, as well as immunomodulatory drugs, are used.
Arbidol can be used as an antibiotic, Acyclovir as an antiviral, and Viferon as an immunomodulator.
Prevention
Since the development of lymphadenitis is caused by a primary disease, the main measure to prevent inflammation of the lymph nodes is timely diagnosis and treatment of the primary pathology. Other preventive measures:
- prevention of injury, in case of injury - timely sanitation (skin damage is treated with iodine, sealed with adhesive tape or bandages are applied);
- teaching the child to observe the rules of personal hygiene;
- careful care of young children;
- general strengthening measures: proper nutrition, covering age-related needs, routine vaccinations, daily walks in the fresh air, active lifestyle, hardening.
Video from YouTube on the topic of the article: