An increase in the level of platelets in a child's blood or thrombocytosis is often detected accidentally during a blood test for other diseases or during a preventive examination. Platelets begin to work when a blood vessel is damaged, participating in the formation of a blood clot and stopping bleeding.
An increase in the number of platelets leads to thickening of the blood and the formation of microthrombi, which clog blood vessels and prevent blood flow. Thrombocytosis is not an independent disease, but one of the signs that requires a thorough examination.
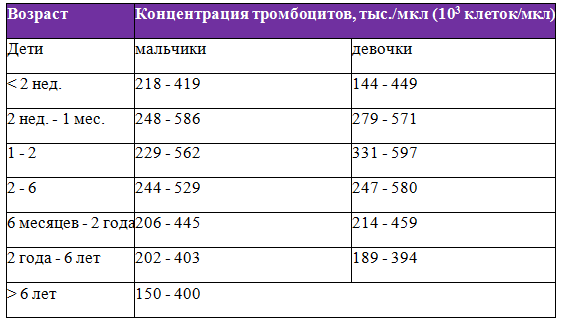
Norms of platelets in the blood of infants from birth to one year
A newborn baby has a higher platelet level than children of other age groups. This is due to the fact that after birth the child enters an environment containing a large number of microorganisms.
During the first month of life, physiological mechanisms are launched in the newborn’s body aimed at eliminating postpartum stress and adapting to environmental conditions. The functional activity of platelets decreases, and more of them are needed to maintain the normal functioning of the blood coagulation system.
| Age | Indicator at 109/l |
| Newborn | 180-490 |
| 1 month | 180-400 |
| 6 months | 180-400 |
| 1 year | 180-400 |
About the normal platelet count in a child’s blood
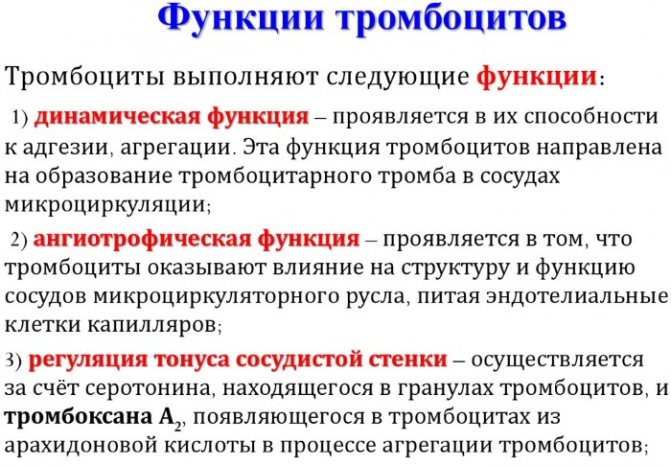
The number of platelets in the body is constantly changing - these blood cells live only 7-10 days, then they are destroyed in the internal organs (mainly in the spleen and liver), and new ones are produced to replace them. The production of platelets is a constant and continuous process. Some cells are destroyed, new ones appear. Even within one day, the amount of these elements may change, but the difference will be no more than 10%.
The following indicators are the norm:
| Child's age | Blood platelet volume |
| 1-9 days | 100-420x10 to the 9th degree l |
| 10 days | 150-400x10 to the 9th degree l |
| 1 month | 160-400x10 to 9 degrees l |
| 6 months | 180-400x10 to 9 degrees l |
| 1 year | 180-400x10 to 9 degrees l |
| 2-4 years | 180-400x10 to 9 degrees l |
Minor deviations from the norm are possible, but since the permissible range is quite wide, if you go beyond its limits, you should still pay increased attention to the child’s health.
If the baby is in good health and rarely communicates with doctors, for control it is enough to take a CBC test to check the number of platelets in the blood once every six months.
Increased platelet count - thrombocytosis
This phenomenon requires treatment, adjustment of the body’s functioning in order to reduce platelets. Otherwise, the colorless bodies will aggregate into large clots, which slows down the blood flow and also leads to the formation of blood clots. And although blood clots in newborns break off extremely rarely, it is better to try to eliminate the likelihood of this process.
Children are most susceptible to thrombocytosis during periods of active growth and stressful situations.
Obvious symptoms of the disease are:
- A bluish tint to the body.
- Pain in the limbs.
- Bleeding gums.
- Enlarged spleen.
Of course, these symptoms may not be related to thrombocytosis, but if at least one of them is present, it is a priori necessary to take a blood test. There are two types of the disease.
Primary thrombocytosis
Increased platelet counts in infants can be caused by dysfunction of the bone marrow, namely, increased division of the primary (parent) platelet cell. This can be caused by heredity or the degeneration of the parent cell from a platelet into a tumor substance. This phenomenon occurs in the following diseases:
- lymphoma;
- lymphogranulomatosis;
- myeloid leukemia;
- erythermia.

Secondary thrombocytosis
Appears when the production of thrombopoietin, an activator of cell division, increases. Or when there has been significant blood loss - in this way the body tries to make up for the platelet deficiency. Secondary thrombocytosis occurs in the following cases:
- infection of the body;
- autoimmune disease;
- injury;
- prolonged bleeding;
- undergone surgery;
- splenectomy;
- chronic kidney disease;
- osteomyelitis;
- tuberculosis;
- anemia (lack of iron in the body);
- hemolysis (excessive breakdown of red blood cells).
Elevated platelets in an infant without an obvious reason require additional research to understand why their number has increased and what this can lead to. It is necessary to treat not only the consequence (which is thrombocytosis), but also the root cause - otherwise the effect on the body will not be effective.
Treatment of thrombocytosis is complex. It consists of taking medications that stabilize hematopoiesis, as well as a balanced diet dominated by dairy products, red meat, red fruits and vegetables, and sea fish. Nuts and seafood are also recommended for adults, but such components are not recommended on the menu for children in their first year of life due to increased allergenicity. It is also necessary to take multivitamin complexes, in which B vitamins predominate.
Rules and technologies for passing analysis
Elevated platelets in a child can be determined using a clinical blood test. There is no separate study to determine their level, since not only the number of platelets is of diagnostic importance, but the counting and comparison of their level with all the formed elements of the blood.
Blood is collected by pricking the ring finger of the left hand. In newborns, blood is taken from the big toe, since the fingers on the hand are very small. Some laboratories take blood from a vein to test platelets.
This is usually done if venous blood is needed for other laboratory tests, such as blood chemistry tests. The examination is performed using an automatic analyzer or using microscopy.
Almost all modern laboratories are equipped with automatic analyzers. Blood testing by microscopy of a drop of blood is carried out when there is a suspicion of a defect in the result of the analysis performed by an automatic method. To determine platelets by microscopy, a drop of blood is smeared on a glass slide and the number of platelets is counted in relation to 1000 red blood cells.
Submission of analysis
In children over 3 years old, blood is taken from a finger or vein for analysis. Biomaterial is taken from the newborn's heel. The examination does not require special preparation, but when donating blood you must follow the following rules:
- The laboratory is visited on an empty stomach. Drinking a small amount of liquid is allowed. Blood is taken from infants 2 hours after feeding.
- The day before the test, physical and psycho-emotional stress is completely eliminated. Hypothermia, walking in hot weather, or taking a warm bath can contribute to changes in coefficients reflecting blood quality.
- Discontinuation of certain medications. The administration of antibacterial or hormonal agents can affect test results. Discontinuation of treatment should be agreed with your doctor.
Important information: The norm of leukocytes in the blood during pregnancy in the 2-3 trimester
If the platelet level in children is too high, it is necessary to repeat the test after a week. The result can be obtained on the day of the test. In some cases, urgent research is required. Indications for determining the platelet level in the blood are the following pathological conditions:
- systemic vasculitis and other autoimmune lesions;
- proliferation of spleen tissue;
- oncological diseases of the hematopoietic system;
- Iron-deficiency anemia;
- acute viral infections.
How long to wait for results, decoding answers
The timing of obtaining a blood test depends on the place of blood donation and the workload of the laboratory. In any case, the analysis result is ready on the same day.
In case of emergency, a blood test can be ready within an hour, and when tested on an automatic analyzer, the test result will be ready in 15-30 minutes.
Could improper blood collection cause abnormal platelet levels?
Failure to comply with the blood sampling rules may result in incorrect interpretation of the test result.
For a reliable study, it is necessary to follow the rules for preparing for blood collection:
- On the eve of blood sampling, you should limit activities associated with increased sweating: playing sports, going to the bathhouse, playing in a stuffy room or in the sun.
- In the evening, exclude fatty and sweet foods from your diet.
- Blood sampling is performed in the morning on an empty stomach. For an infant, blood can be drawn 2 hours after feeding.
- The analysis must be taken before X-ray examination, massage, physiotherapy and taking medications.
- Before taking a blood test, it is necessary for the child to sit quietly for 10 minutes.
- If a follow-up study is necessary, the test should be taken in the same laboratory.
Causes of increased platelets in the blood of a child
Elevated platelets in newborns are detected in 13% by 1 month. this figure increases to 36%. By 6-12 months. the frequency of thrombocytosis decreases and is the same as in newborns. Upon re-examination, in 50% of cases, platelets decrease to normal levels.
There are familial, primary or clonal and secondary or reactive thrombocytosis.
Cases of familial thrombocytosis are very rare. The main cause of familial thrombocytosis is a mutation of the gene that is responsible for the production of thrombopoietin, a regulator of platelet production.
It is impossible to distinguish between primary and secondary thrombocytosis by determining platelet levels. Extreme thrombocytosis can occur both in patients with cancer and with inflammation of the intestines or kidneys.
The incidence of primary thrombocytosis is 10% of all detected platelet count disorders. Primary thrombocytosis occurs in tumors of the hematopoietic system due to an increase in the number of megakaryocytes, which are precursors of platelets.
This is a group of myeloproliferative diseases which include:
- Chronic myeloid leukemia. With this disease, the number of leukocytes increases, up to the appearance of young forms and blast cells, sometimes eosinophils and basophils increase. An increase in platelets does not always occur.
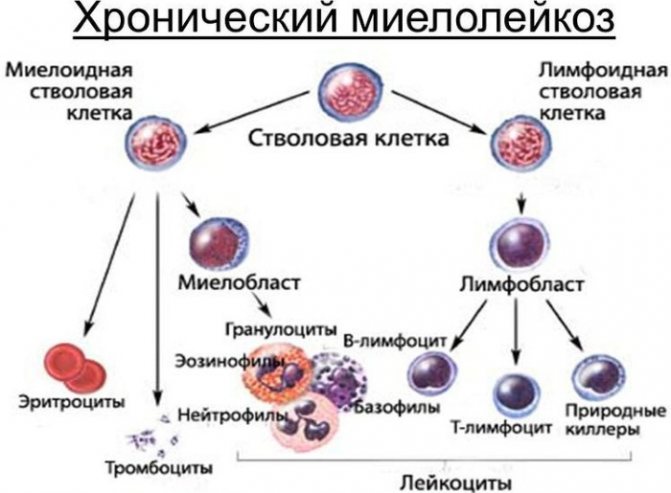
- Polycythemia vera. The disease is characterized not only by an increase in platelets, but also in hemoglobin, red blood cells and sometimes white blood cells.
- Idiopathic myelofibrosis. With this pathology, against the background of an increase in platelet levels, there is a decrease in hemoglobin levels and an increase in the number of leukocytes. Thrombocytosis is caused by increased production of systemic anti-inflammatory factors that stimulate platelet production.
- Essential thrombocythemia. This pathological process is characterized by isolated thrombocytosis without changes in other blood parameters. The clinical picture of the disease is characterized by episodes of thrombosis or bleeding.
If a myeloproliferative disease is suspected, in order to clarify the diagnosis, a bone marrow examination for cytogenetic research is necessary.
Secondary thrombocytosis occurs in acute conditions accompanied by massive blood loss, trauma or extensive surgery. In this case, thrombocytosis is a compensatory condition due to the body's response to a decrease in circulating blood volume.
An increase in the number of platelets in children occurs with long-term chronic diseases, which include:
- Iron deficiency anemia - occurs due to nutritional deficiency; for conditions requiring increased iron consumption (pregnancy and lactation); for chronic bleeding (menorrhagia, bleeding from the gastrointestinal tract). The main diagnostic criterion is a decrease in serum iron and ferritin levels. Thrombocytosis appears with chronic and long-term anemia.
- Infectious inflammatory diseases are one of the most common causes of thrombocytosis in children. Inflammatory diseases can be bacterial, viral or fungal in nature (pneumonia, meningitis, pyelonephritis, enterocolitis). In inflammatory diseases, platelets play a role in neutralizing pathogenic microorganisms. With a decrease in inflammatory manifestations, along with an improvement in other laboratory parameters, the number of platelets decreases.
- Chronic autoimmune diseases : rheumatoid arthritis, systemic lupus erythematosus, periarteritis nodosa, scleroderma - with these diseases there is an increased production of inflammatory factors that activate platelet production.
- Solid tumors are malignant, rapidly progressing formations that develop from the epithelial tissue of the lungs, liver, kidneys, thyroid gland and other organs. The increase in platelets is due to the fact that the tumor tissue produces substances that help increase platelet production.
- Condition after removal of the spleen. The spleen is the organ where platelet destruction normally occurs. After surgery, the maximum level of platelets in the blood appears after 1-3 weeks and persists for a month.
- Asplenia - a congenital pathology in which the spleen is absent. Asplenia occurs very rarely, mainly in boys, and is accompanied by developmental abnormalities in other organs.
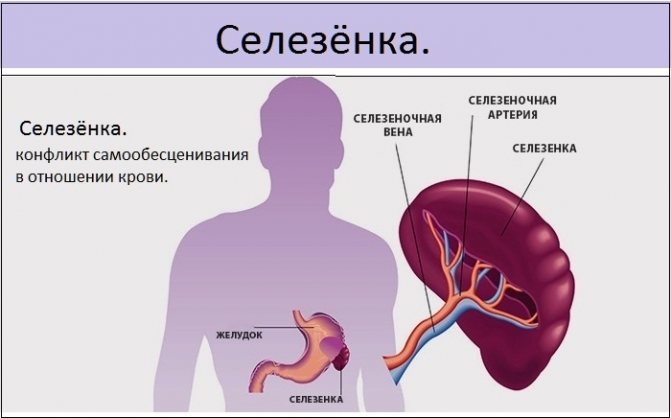
The cause of an elevated platelet level in a child may be the absence or disease of the spleen. - Thrombocytosis may be due to a side effect of certain medications. When treated with corticosteroids (prednisolone) and sympathomimetics (adrenaline), which are used in the treatment of allergic diseases, an increase in the number of platelets is possible. Long-term use of vitamin B12 and folic acid can also cause thrombocytosis.
Reactive thrombocytosis is caused by activation of platelet precursors in the bone marrow. Reactive thrombocytosis is a benign condition and is easily treated because, despite the increase in the number of platelets, their size and function remain unchanged. The diagnosis of secondary thrombocytosis is not difficult and is based on the symptoms of the underlying disease.
There is a concept of physiological thrombocytosis. These are conditions in which an increase in platelet levels is not a sign of disease.
Occurs when:
- Overexcitation of the nervous system.
- After physical activity.
- When dehydrated.
False thrombocytosis - occurs when a blood test is incorrectly interpreted when examined on an automatic analyzer, when small particles are regarded as platelets:
- Small red blood cells in microcytic anemia.
- Cytoplasm of destroyed blast cells during chemotherapy in cancer patients.
- Bacteria in the blood.
- Cryoglobulins are blood proteins that appear in autoimmune diseases and tumors.
Normal value
From birth until adolescence, platelet distribution levels will change. After a year, the number of platelets in the blood will gradually return to the levels for an adult.
Norm of platelets in the blood of children by age (table):
| Age | Platelets normal |
| In newborns | 180–490 |
| Platelets in a baby in the first month | 180–400 |
| Up to a year | 180–400 |
| From one year to 2 years | 160–390 |
| 3 years | 160–390 |
| 4 years - 5 years | 160–390 |
| From 6 years to 10 years | 160–380 |
| During adolescence (13–15 years old) | 180–320 |
The average platelet volume is 180–380 units. A slight deviation in the indicators is acceptable - by 1-2 units.
Signs of a high platelet count
Elevated platelets in a child do not manifest themselves clinically. Signs of thrombocytosis are nonspecific and can often be identified only after examination.
However, if your child develops the following symptoms, you should consult a doctor:
- Weakness, fatigue, decreased performance.
- Headache, dizziness.

- Decreased background mood.
- Numbness and tingling in the extremities with a feeling of constant coldness in the arms and legs.
- Increased blood pressure.
- Peripheral edema.
- Dryness and itching of the skin.
- Nosebleeds and formation of hematomas on the skin.
Elevated platelets in a child, if detected by chance and in the absence of specific complaints, require re-examination after 5-7 days. In 50% of cases, the second analysis does not detect changes in the platelet count.
If thrombocytosis persists, examination is required to identify the disease that may be causing it. Additional examination methods are also necessary for the differential diagnosis of thrombocytosis.
- Blood chemistry. With secondary thrombocytosis, inflammatory markers increase: C-reactive protein, fibrinogen, ESR. Primary thrombocytosis and tumor diseases of the blood are characterized by an increase in lactate dehydrogenase. With anemia, ferritin and serum iron decrease.
- A coagulogram reveals disorders in the blood coagulation system.
- Ultrasound of internal organs is an examination method that can be used to identify space-occupying formations if a tumor is suspected. In thrombocytosis, special attention should be paid to the size of the spleen.
- X-ray of the chest organs to identify an inflammatory process in the respiratory organs or identify a tumor formation.
- trephine biopsy is performed for primary thrombocytosis to identify the form of the disease.
- Molecular genetic examination of blood and bone marrow to exclude genetic pathology.
How to lower the platelet count in a child's blood
Elevated platelets in a child are not an independent disease, but a secondary complication of other diseases, so treatment will be aimed directly at the main cause of the disease and preventing complications.
Medicines
Drug treatment is the main way to reduce platelets in the blood.
Medicines are prescribed depending on the underlying disease that caused thrombocytosis:
- For primary thrombocytosis, the main treatment method is cytostatics - drugs that suppress the growth of platelet precursors: mercaptopurine, cytarabine, hydroxyurea.

- Anagrelide is the drug of choice for essential thrombocythemia. The drug affects the function of thrombopoietin, which is the main regulator of platelet production.
- Interferon alpha - suppresses the sprouts of hematopoietic tissue.
- To prevent the formation of blood clots, antiplatelet agents are used - drugs that prevent platelets from sticking together and forming a blood clot. These medications include: acetylsalicylic acid, clopidrogel, trental, pentoxifylline.
- Anticoagulants – prevent the formation of blood clots and prevent an already formed blood clot from enlarging: heparin, warfarin, fraxiparin.
- If a blood clot has already formed, then thrombolytics are used: streptokinase, urokinase.
Nutrition
Since the main complication of an increased level of platelets in the blood is its thickening and the formation of blood clots, it is necessary to consume products that help thin the blood. If a similar condition occurs in a breastfed child, then in addition to basic nutrition, the child should be supplemented with water between feedings.
Increasing the drinking regime helps thin the blood. Only clean water is suitable for drinking, the volume of which is 30 ml/kg per day. Older children should exclude sweet juices and carbonated water from their diet, which can thicken the blood due to the large amount of sugar.
In your diet, you should limit the consumption of foods high in carbohydrates (porridge, flour products, bananas, potatoes). Substances that help thin the blood include vitamins E, B6, C, so foods with a high content of them are included in the main diet:
- Seafood (fish, seaweed) contains omega-3 polyunsaturated fatty acids, taurine, iodine, which prevent blood from thickening and promote the resorption of existing blood clots.

- Olive, flaxseed, and sea buckthorn oils are also a source of omega-3 polyunsaturated fatty acids.
- Fruits (lemon, tangerines, oranges, apples) contain large amounts of vitamin C, which helps thin the blood. You can take freshly squeezed juices diluted with water by half.
- Vegetables as a source of fiber will be beneficial in increasing platelet counts. Tomatoes, which contain the substance lycopene, deserve special attention. It reduces blood clotting and reduces thrombus formation.
- Spices: onion, garlic, ginger, turmeric, cinnamon reduce blood viscosity.
Additional therapy methods
If surgical treatment is necessary in persons with myeloproliferative diseases, a plateletpheresis procedure is performed to quickly reduce platelets. Thrombocytapheresis is a procedure for taking blood from a patient and then separating platelets by centrifugation on an automatic apparatus for separating blood cells.
The procedure is carried out in several stages:
- A sterile needle is used to puncture a vein located in the elbow area.
- The needle is connected using a special system to the separation apparatus.
- An automatic blood draw is performed.
- The device separates platelets from other blood elements.
- The platelet-free blood is returned to the patient through a vein in the other arm.
For patient safety, blood is drawn in a small volume. The entire procedure takes about 1 hour.
Test to determine the level of platelets in the blood
What tests can be prescribed, including counting platelet levels in the blood? One of these tests is a general clinical blood test. This is a study of the level of red blood cells, white blood cells and platelets together. Depending on the equipment the laboratory is equipped with, other blood parameters may be determined.
Most often, a hematology analyzer is used for general clinical blood analysis. Therefore, there are a number of factors influencing the reliability of the results.
Sometimes, if the indicators are inadequate or questionable and do not correspond to the clinical picture, a separate study of platelet levels may be prescribed. It is carried out manually, and in this case it is more reliable, as it helps to avoid erroneous readings from the device.
Complications of high platelet levels in the blood
When platelets increase to 1000 x 109/L, there is no risk of complications such as thrombosis or bleeding. When platelets exceed this value, there is a risk of thrombohemorrhagic complications.
The main complications with an increase in platelets in the blood are caused by an increase in blood viscosity and a tendency to increased thrombus formation.
- Increased blood pressure. Due to the high viscosity of blood, it is more difficult for the heart to push it through the vessels. The heart begins to work harder and blood pressure increases.
- Low blood flow speed leads to a lack of nutrition in the internal organs, hypoxia develops due to lack of oxygen, which leads to increased fatigue and headaches.
- Bleeding from superficial vessels of the skin, mucous membranes, stomach, urogenital tract.
- Due to the large number of platelets, they stick together and form blood clots that clog veins or arteries. Venous thrombosis in children is very rare. The clinical picture of thrombosis depends on its location. For example, with thrombosis of the femoral vein, swelling and pain appear in the lower limb. Arterial thrombosis is also an extremely rare complication in children. There may be an ischemic stroke of the brain or a transient ischemic attack due to the cessation of blood flow to any area of the brain. The clinical picture depends on the location of the stroke.
An increase in the level of platelets in the blood is a common pathology in children, which in most cases goes away on its own or after treatment of the underlying disease. With persistent thrombocytosis, even in the absence of complaints, there is a risk of detecting oncohematological diseases.
Article design: Vladimir the Great
Assessing blood platelet levels
Main article: Find out everything about platelet levels in children
To obtain the most accurate test results, the platelet level in a blood test must be determined on an empty stomach. Also, before taking blood, it is necessary to avoid physical or emotional stress.
You can drink water before blood collection.
For emergency indications (acute blood loss, dehydration due to vomiting, diarrhea, etc.), blood sampling is carried out at any time of the day, regardless of the last meal, etc.
Normally, the level of platelets in the blood varies depending on the gender and age of the patient. Age and gender fluctuations in the normal limits are observed up to six years. Subsequently, platelet cell levels do not differ between women and men.
The limits of normal platelet cells in children are presented in the table: