Pregnancy is one of the happiest periods in a woman’s life, but not every expectant mother can enjoy it. If a pregnant woman has a negative blood type, and the child inherits a positive Rh father, the risk of Rh conflict is very high, which increases by 10 percent with each subsequent pregnancy.
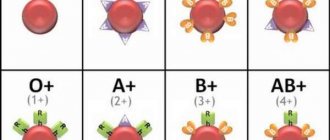
The essence of the Rh conflict is as follows. Human red blood cells may contain a protein called the Rh factor. If it is present, they say that the Rh factor is positive; if it is absent, then it is negative. If a child is conceived from parents with different Rh factors, a Rh conflict occurs - a phenomenon in which the woman’s immune system perceives the fetus as something foreign that can cause harm to health, and tries to get rid of it. This increases the risk of miscarriage, premature birth, and hemolytic disease in the newborn.
To avoid terrible consequences and help a woman bear and give birth to a healthy baby, doctors recommend administering immunoglobulin during pregnancy to patients with a negative Rh factor.
The role of injections during pregnancy
Immunoglobulin is a special protein fraction consisting of antibodies that were obtained from donor blood plasma. Antibodies are produced by lymphocytes when foreign agents enter the body. Their function is to attack pathogens and destroy them.
Medicines containing immunoglobulin are of two types.
- Human. It is used when faced with various infections, such as herpes. This type of remedy is usually not recommended during pregnancy, however, they are resorted to if antibacterial agents are powerless and the likelihood of miscarriage is high. The drug is used to stimulate the immune system.
- Anti-Rhesus. A medication intended for use in case of Rh conflict.
The difference between these types of medication is that the latter (anti-D immunoglobulin) consists of antibodies to positive Rh antigens, and not any of the viruses.
When immunoglobulin is administered during pregnancy, the antibodies it contains replace maternal immune cells. Positive red blood cells that enter her blood from the fetus are destroyed, thereby preventing abortion. Timely injection of the substance will allow you to carry the baby to term normally and significantly reduce the risk of developing hemolytic diseases in the second and subsequent children.
Indications and contraindications for use
Anti-Rhesus immunoglobulin during pregnancy is prescribed only to women with Rh negative, provided that the future father is Rh positive. The injection will be given in the following cases:
- during the period of bearing a baby;
- at the birth of a child with a positive Rh factor (this is determined by a blood test);
- after a miscarriage or abortion;
- after an ectopic or non-developing pregnancy;
- if there is a threat of interruption at any time;
- after any invasive procedures, in particular amniocentesis;
- for abdominal injuries.
The drug is scheduled to be administered at the 28th...30th weeks of pregnancy and within three days after the baby is born (if it is confirmed that the child has inherited the paternal rhesus). We can conclude that such a procedure is an immunoglobulin vaccination that prevents future Rh conflict.
Emergency injection of immunoglobulin is indicated for the prevention of Rh conflict in case of spontaneous miscarriage, placental abruption, and premature birth.
There are situations in which serum cannot be administered:
- high sensitivity to the components of the product;
- allergic reactions to any blood products;
- negative Rh factor, accompanied by sensitization and the presence of antibodies in the blood;
- Rh positive.
Rhesus conflict in the womb
Erythrocytes—red cells—circulate in human blood. In most people, a protein antigen “lives” on the surface layer of red blood cells, which is called the Rh factor; If there is such an element, it means that the person has Rh-positive blood. When no protein is detected on red blood cells, the blood is considered Rh negative.

The presence or absence of a protein called Rh factor divides people into Rh positive and Rh negative.
Approximately every seventh inhabitant of the planet has an Rh negative factor. During surgical operations, this indicator is extremely important - if “positive” blood is mixed with “negative”, the person will die.
In ordinary life, a negative Rh factor does not affect health, including mental activity; people play sports - extreme sports too - experience other physical activities, make scientific discoveries, and so on. If only in case of severe injuries they notify doctors in time about their Rh factor.
Problems begin for a number of women after conceiving a child.
Imaginary threat
So, pregnancy came. A woman has Rh-negative blood, a man has Rh-positive blood. There is a 50% chance that the unborn child will inherit his father’s blood level. As a result, for maternal antibodies the baby turns into a foreign object - they also discovered an element unfamiliar to them in the fetus - the Rh factor.
From 20 to 29 weeks of pregnancy, an urgent mobilization is announced in the female body: antibodies are intensively produced to eliminate the small “enemy”. An attack by the adult immune system threatens to be fatal for the fetus - its immune system is not yet capable of adequate protection. As a result, the child’s red blood cells stick together and then are destroyed, which leads to the following consequences:
- freezing of the fetus in the womb (actually death);
- premature birth;
- hypoxia (oxygen starvation) of the fetus;
- a child is born with a hemolytic disease, the consequences of which are severe anemia (anemia), damage to the heart, liver, deafness, and paralysis.

occurs due to dysfunction of the liver. Scientists have yet to find out why such a “blood feud” is not typical for different blood groups - for example, the mother has group 1, the father has group 4, but the child develops normally. It is assumed that the Rh factor as an evolutionary trait historically appeared not so long ago and nature has not yet developed a mechanism for “warring systems” to adapt to each other.
How does anti-Rhesus immunoglobulin work?
The main task of the drug is to prevent the formation of antibodies that attack elements of the baby’s Rh-positive blood. More precisely, there is one element - antigen D, and maternal immune cells take up arms against it; other rhesus antigens do not cause such an aggressive reaction.
Anti-Rhesus immunoglobulin is saturated with antibodies designed to fight D antigens - that is, at first glance, there is no better way to “kill” the fetus completely. However, something else happens - the substances from the drug seem to “calm” the woman’s immune system: everything is in order, we have come to help, there is no need to produce our own antibodies, rest, please. And it works - the maternal immune system, deceived by the medicine, does not think of creating immunoglobulins to destroy the fetus. Replacement therapy gives the first result.
Meanwhile, the antibodies from the drug, unlike maternal antibodies, are not able to penetrate to the fetus - and this is another plus.
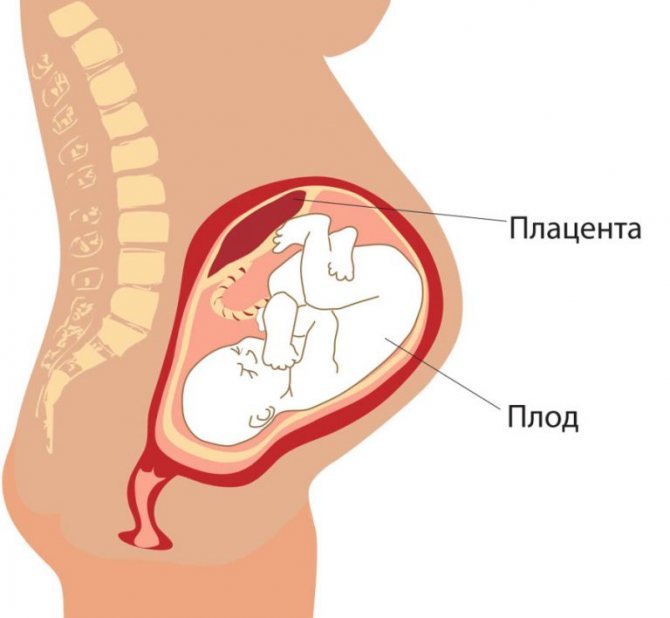
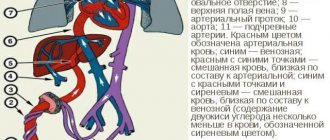
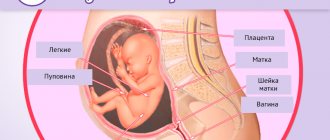
The placenta is a temporary organ that blocks the path of immunoglobulins from the drug to the fetus
Over time, medicinal substances are gradually eliminated from the body—accumulation is not expected. And your own antibody production is blocked. Thus, anti-Rhesus immunoglobulin, acting on the principle of “white lies,” deceives the unwitting aggressor and saves the fetus.
Who needs medicine first?
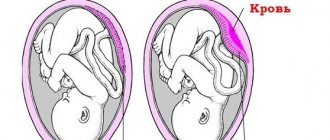
The blood circulation of the mother and the fetus are two separate systems; ideally, both blood flows do not mix until blood with D antigens of the unborn baby suddenly ends up in the mother’s body. Once in “enemy territory,” fetal red blood cells stimulate women’s immunity to produce immunoglobulins. With the bloodstream, antibodies penetrate through the umbilical cord to the baby and begin their destructive work.
Fetal D antigens appear in maternal blood if:
- the woman previously had an abortion at a period of more than 8 weeks, when the fetus had already begun to produce its own red blood cells; then, during termination of pregnancy, they penetrate the woman’s blood and provoke the synthesis of antibodies;
- previous pregnancy ended in miscarriage after 8 weeks;
- an operation was performed to stop an ectopic pregnancy;
- the woman received a penetrating injury or bruise to the abdomen;
- in a pregnant woman, the functions of the placenta are impaired - fetoplacental insufficiency is observed, which is accompanied by a disruption of normal blood flow, or partial placental abruption, leading to the same thing;
- before delivery, amniotic fluid began to leak;
- the woman underwent amniocentesis (diagnostic procedures with invasive intervention) - as a result, fetal tissue was inadvertently injured; such procedures should be performed only in cases of extreme necessity and invariably accompanied by treatment;
- the previous pregnancy ended successfully with the birth of a baby.
Such expectant mothers with “negative” blood are included in the risk group; The doctor prescribes an injection of anti-Rhesus immunoglobulin to a woman.
During a successful first pregnancy, of course, you need to be on guard, but the likelihood of Rh conflict is minimal, so you can do without the drug. Maternal immunity produces antibodies, but they are too large to pass through the placenta or umbilical cord to the fetus. During childbirth, the situation changes radically: the child’s blood inevitably mixes with the blood of the mother in labor, the mother’s immune cells sound the alarm, and the mechanism for producing antibodies is launched, which rushes to attack “strangers.” The D antigens have been destroyed, but the baby is already outside the womb and therefore safe.
Problems come with the second pregnancy. Maternal antibodies are already on alert, and if the embryo has a positive Rh factor, the danger of conflict increases. Nothing will change the situation: having once produced antibodies to D antigens, the female body has forever “written down” this Rh factor as an enemy and is henceforth doomed to fight.
After the first birth, to prevent Rh conflict from occurring during subsequent pregnancies, the woman is given an injection of anti-Rhesus immunoglobulin.
According to statistics, with each pregnancy of a Rh-negative mother, the likelihood of a “war” with D antigens, and therefore a threat to the health, and even the life of the unborn child, increases by 10%. However, the risk to the fetus is reduced to zero when it has inherited a negative Rh factor.
To make sure that she has a Rh conflict, the expectant mother takes a blood test for antibodies - first after 7 weeks, then at 20 weeks; before giving birth you have to go for tests every week. An ultrasound will also show that something is wrong: the placenta is thicker than normal, there is too much fluid in the abdominal cavity.
By increasing the level of the coloring protein bilirubin in the blood, doctors judge the severity of the Rh conflict, since bilirubin shows how destroyed the red blood cells are.
Video: doctors talk about Rh conflict in a pregnant woman
Which immunoglobulin is better during pregnancy?
The most common medication option, as well as the most affordable, is Normal Human Immunoglobulin. It has many analogues, for example:
- Gamimun N;
- Gamunex;
- Gabriglobin;
- Pentaglobin;
- Immunovenin;
- Intraglobin.

The main difference between all drugs is their cost. Normal immunoglobulin costs about a thousand rubles, while Immunovenin costs about three, and Gabriglobin costs almost seven thousand rubles. Anti-Rhesus immunoglobulin will cost the same amount. However, a pregnant woman does not have to worry, since these drugs are purchased centrally, and if indicated, the injection will be given absolutely free.
It is impossible to say which medicine is better, since their mechanism of action is similar, and the compositions are the same. Only prices and manufacturers differ.
How the drug is administered
The planned administration of the serum is carried out on time in the antenatal clinic as part of prenatal prevention. The second injection will be given in the maternity hospital if the baby is Rh negative.
If there is a threat of miscarriage, the pregnant woman is prescribed one average dose of medication in a hospital or antenatal clinic.
After a miscarriage or abortion, as well as an ectopic pregnancy, immunoglobulin should be administered immediately after completion of the operation.
If immunoglobulin is administered urgently, then its dosage is calculated on the spot and does not depend on the amount of fetal blood mixed with the maternal one. This usually occurs after injury or invasive procedures.
In all of these cases, the drug is injected deep into the muscle. Immediately before injection, the product should be warmed to the patient’s body temperature. You should not listen to erroneous information on the Internet that the drug is indicated for drip injection. Intravenous administration of immunoglobulin is not provided and is contraindicated.
Are there possible side effects and overdose?
The vaccine has been effectively used to prevent Rh disease since 1968. Since then, no severe reactions to the medication have been recorded. There is also no information about overdose. However, some side effects still sometimes make themselves felt.

Consequences for the mother
Side effects of immunoglobulin for the expectant mother manifest themselves as follows:
- local reactions similar to allergic ones. Anaphylactic shock syndrome occurs very rarely;
- infection. Serum is an extract from donor blood. It is unknown what diseases the donor suffered from, but manufacturers claim that the drug is carefully purified. In addition, donors are screened before donating blood;
- risk of overdose. It is very insignificant.
Sometimes pregnant women complain of headaches, fever, nausea and dizziness. Usually these unpleasant symptoms go away quickly. To be safe, it is better to remain under medical supervision for some time (at least half an hour).
Is vaccination dangerous for the fetus?
The injected substance quickly penetrates into the fetal blood, overcoming the placental barrier. Thus, the baby’s passive protection from infections and other threats begins. Interestingly, human immunoglobulin is able to protect a child from infections that his mother has never even encountered.
The medication does not negatively affect the baby’s body.
Consequences of taking anti-Rhesus immunoglobulin
The drug is considered safe for mother and fetus, although there are not enough clinical trials to confirm this opinion. They rely on reviews from women who were injected with the product. In the body, the medicine will destroy the D antigens that got there with the child’s Rh-positive blood - anyway, they will not take root; but the production of aggressor antibodies is temporarily suppressed. There are also no threats to the baby - the placental barrier will not allow immunoglobulins from the medicine to pass through. As a result, both the pregnancy and the health of the fetus were saved.
Injections of the solution do not conflict with taking other medications; The use of antibiotics is also permitted.
Contraindications
There are almost none for pregnant women. It has already been said that the drug will not help those Rh-negative expectant mothers who have their own Rh antibodies in their blood serum.
In addition, there are women with increased sensitivity to human immunoglobulin - after all, it was obtained from someone else’s donor and, given the widespread allergies that have swept the world, it is quite capable of causing a negative reaction in a pregnant woman. This happens in exceptional cases, but incidents have been recorded in which women experienced anaphylactic shock after administration of the drug. That is why the procedure is done in a medical facility where it is possible to carry out anti-shock therapy.
When the patient knows that she cannot tolerate immunoglobulin, she has to look for other methods of therapy.
In general, the medicine has been used for exactly 50 years - the first injections of anti-Rhesus immunoglobulin were made back in 1968. The drug has a good reputation thanks to a lot of positive reviews from doctors and patients.
Adverse reactions
Alas, a “side-effect” is not excluded. Occasionally the injection is accompanied by:
- an increase in temperature to 37.5° in the first 24 hours; Considering that Rh-negative people live with a slightly lower body temperature, such an increase for them seems significant;
- heaviness in the stomach, difficult digestion;

After an injection of anti-Rhesus immunoglobulin, the expectant mother may feel an unpleasant heaviness when she eats - redness of the skin (with mild allergies).
In one out of ten thousand cases of drug administration, the patient becomes infected with AIDS or hepatitis. Despite the careful monitoring of donor blood declared by the manufacturers, the factor of negligence plays its evil role.
Doctors exclude the risk of overdose: the instructions for the drug clearly indicate the dosage for different cases.
Interaction with other drugs
Anti-Rhesus immunoglobulin does not interact with other pharmaceuticals; it can be administered simultaneously with antibiotics or hormonal agents without any problems, the main thing is to follow the recommended timing. However, it should not be mixed in the same syringe with other medications.
Reviews from women who received immunoglobulin for Rh-conflict are mostly positive. No one complained about the occurrence of complications during the planned administration of serum during pregnancy (as part of prophylaxis before labor), or after childbirth. No cases of hemolytic diseases in children have been recorded. However, some patients stated that the doctor obliged them to pay for the drug. This is normal if pregnancy care is carried out in a private clinic. But in public medical institutions, such a practice is unacceptable and illegal, since anti-Rhesus immunoglobulin is included in the list of vital drugs. This means that women who are registered with a gynecologist at the antenatal clinic under the compulsory medical insurance policy do not need to pay for the injection. It is important to know about this and not to be deceived.
Opinions of doctors and patients
Some doctors argue that the administration of immunoglobulin is the only way to save the fetus in case of Rhesus conflict. Others do not advise using the drug during pregnancy, since it has not undergone enough testing that could confirm its effectiveness. Serum for injection can lead to the side effects described above and only worsen the condition of the expectant mother. In exceptional cases, the use of serum leads to dangerous side effects, such as tachycardia (Analgin with Diphenhydramine has worked well in the fight against it), fainting, and anaphylactic shock.
There were situations when the medicine increased the production of antibodies in the body of a pregnant woman and the Rh conflict remained. Self-therapy is strictly prohibited, as it can lead to serious complications. Before determining the dosage, the doctor conducts tests to understand the degree of Rh conflict.