Why are platelets needed?
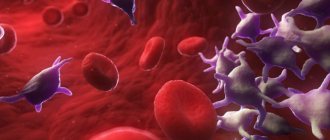
Another name for platelets is platelets (or Bizzocero plaques). These cells received this name due to their structure.
A platelet is a small plate, the size of which does not exceed 1.5-4 micrometers, separated from a megakaryocyte (a large cell that makes up bone marrow tissue).
The shape of the body plate is maintained by microscopic tubes located along the entire perimeter of the cell. The content of platelets in the blood averages from 60 to 75% of the total, the remaining part (approximately 25-40%) accumulates in the spleen.
The number of platelets in the blood plasma can fluctuate both up and down throughout the day. But these fluctuations should not exceed 10%. If the difference during the day is greater than the specified value, pathology or disturbances in the functioning of internal organs can be suspected.
The main function performed by platelets in the human body is the formation of platelet clots necessary to prevent blood loss and participation in blood clotting processes.
The role of platelets in the functioning of the child’s body
There are several functions that a small organism needs a certain number of platelets to perform. These include:
- restoration of damaged blood vessel cells;
- participation in cell division processes;
- transportation of immune complexes and their attachment to the cell membrane;
- maintaining the contractile ability of vascular walls due to serotonin;
- release of proteins necessary for blood clotting;
- the formation of blood clots (adhesion), necessary to stop bleeding and reduce blood loss.
If a child has a low platelet level, any wound or cut can result in severe bleeding, which is difficult to control at home. To prevent this from happening, it is important to regularly take a general blood test and, if any abnormalities are detected, carry out age-appropriate therapy.
How is the number determined?
To determine how many platelets a child has, a CBC is performed. This analysis is important for all babies. For testing, blood is mainly taken from a finger. Blood may be taken from the infant's heel. PLT in a blood test stands for platelet concentration. The analysis is carried out as planned, i.e. even for healthy children. A mandatory check of platelets in a child’s blood is carried out if he has a disease that can affect changes in the number of these cells.
In order for the analysis readings to be correct, it is necessary to prepare the baby for the procedure:
- You need to donate blood in the morning and on an empty stomach. This affects the rate of platelet formation.
- The last meal should occur 12-14 hours before the procedure.
- Excessive physical activity is prohibited.
- 7 days before the study you must stop taking any medications.
- It is important to mentally prepare the child. Stress affects the production of blood cells.
For a more detailed check of the coagulation system, a coagulogram is used. It is needed to determine the cause of disorders of the circulatory system. In addition, it is carried out before prescribing drugs that affect the functions of coagulation and hematopoiesis. A coagulogram is a comprehensive study that includes the study of 9 to 13 platelet characteristics.
What affects the quantity
Among the diseases affecting the number of platelets in the blood are:
- viral infections;
- anemia;
- diseases of the spleen, liver, thyroid gland;
- leukemia;
- immune pathologies;
- tuberculosis;
- heart failure;
- measles;
- thrombocytopenic purpura syndrome.
Platelets in children are also influenced by heredity. In addition, cell levels may change as a result of medications (as an adverse reaction). In girls, the level of platelet elements in the circulatory system decreases during menstruation, and changes during the day become more chaotic. The cause may be poor nutrition and vitamin deficiency. Doctors often cannot figure out the cause of changes in PLT in the blood.
Average platelet count as the norm for children in the table
The platelet content in a child’s blood depends on many factors, for example, health status, nutritional habits, age, etc. Age is the main criterion when determining compliance with standards.
The normal platelet count depending on the age of the child (the table shows values for healthy children!)
| Age | Blood cell content (per liter of blood) |
| Newborn (1-3 days after birth) | 100-420*109 |
| 7-10 days | 150-400*109 |
| 1 month | 160-400*109 |
| 6 months | 180-400*109 |
| 12 months | 160-380*109 |
| From 1 to 4 years (inclusive) | 160-400*109 |
| From 5 to 7 years (inclusive) | 180-450*109 |
| Over 7 years old | 180-460*109 |
How to determine the level of platelets in the blood?
To determine the volume of blood cells, a general blood test is used, which is done even to newborn children 1-3 days after birth.
For the purpose of early detection of pathologies, healthy children are recommended to donate blood at least once a year.
If there is a hereditary predisposition to the development of thrombocytopenia or thrombocytosis, the pediatrician may prescribe a complete blood count more often, for example, 2-4 times a year. Bone marrow pathologists, as well as some diseases, also require more frequent monitoring.
Do I need special preparation before taking the test?
In order for the analysis to be as accurate as possible, the baby should be properly prepared for blood donation. To do this, you must follow the following rules:
- the fasting period should be at least 8 (for children under 7 years of age) or 12 hours (for children over 7 years of age);
- collection of material should be carried out in the morning (60-120 minutes after waking up);
- Drinking and eating food before the analysis is not allowed (you can give the baby some clean drinking water);
- 1-2 days before donating blood for analysis, it is necessary to limit the child’s physical activity and activity (if the child goes to school, you should skip physical education class);
- Under no circumstances should you rub your fingers before entering the nurse's office, as this may affect test results (for example, white blood cell levels, etc.).
Deviations from the norm
If the platelet count is normal, then the body maintains a balance between the formation and destruction of fragments.
The main function of platelets is to stop bleeding.
A change in the level of these elements leads to weakened blood clotting or increased thrombus formation. A 5-10% change in cell number within 24 hours is considered normal. The level of platelets in the blood also affects the following functions:
- accumulation of substances that accelerate the growth of blood cells;
- getting rid of foreign microorganisms;
- obstacle to inflammatory processes;
- accelerating tissue regeneration by cell splitting.
The lack of an element leads to partial performance of the specified functions. Chaosity increases, because the cells cannot withstand the load and are destroyed. Excess leads to overfulfillment of functions. Blood flow is impaired because clots begin to form throughout the circulatory system.
Thrombocytopenia
When platelets in a child’s blood are low in number, a dangerous pathology begins to develop - thrombocytopenia. This disease has become common in newborns. The disease most often appears in winter or spring. Causes of thrombocytopenia:
- anemia;
- tuberculosis;
- leukemia;
- poisoning;
- acute viral infections;
- severe stress;
- allergic reaction to various foods and medications;
- cirrhosis of the liver;
- Infectious mononucleosis;
- hemolysis.
Important information: What does it mean to shift the leukocyte formula to the left and to the right?
Most often the disease is caused by viral infections, mononucleosis and aplastic anemia. Diseases such as influenza, hepatitis and herpes impair blood clotting. With mononucleosis, the lymph nodes become larger, which causes the spleen to enlarge. Anemia negatively affects the formation of all blood elements.
With thrombocytopenia the following are observed:
- Poor blood clotting.
- Bleeding gums when brushing teeth.
- Frequent bruising due to the thinness of the capillaries.
- Formation of hematomas due to rubbing with clothing.
- The urine becomes red in color.
- Stool with blood clots.
- When eating solid foods, there is a risk of damage to the mucous membrane, which leads to internal bleeding.
Signs and treatment in children and adults are almost the same. However, children are more sensitive to the disease, and their pathology develops faster. The first symptoms are most often nose and mouth bleeding and the appearance of a rash. The rash first appears on the lower extremities and eventually spreads to the child’s arms. There are no painful symptoms, so many do not attach much importance to this.
Thrombocytosis
Manifests itself as an indicator that exceeds platelet standards in children. Children around 6 months of age often have elevated readings, but this does not mean they are sick. Such indicators are caused by increased physical activity and teething.
The primary cause of thrombocytosis is bone marrow pathology. Secondary:
- leukemia;
- infections (acute respiratory infections, influenza, hepatitis);
- allergies to drugs;
- erythremia;
- iron deficiency;
- spleen diseases;
- liver diseases;
- anemia;
- lymphogranulomatosis;
- primary thrombosis.
Thrombocytosis is characterized by severe symptoms, but they appear in the later stages:
- Gums are bleeding.
- The size of the spleen increases.
- Urination is impaired.
- Hematomas appear.
- Bleeding begins from the mouth and nasal cavity.
- Internal bleeding in the digestive organs is possible.
- Discomfort in the kidney area.
- Itching and redness on the skin.
- Insomnia.
- Dizziness.
- Lethargy and apathy.
Important information: Normal ESR in the blood of women by age (table of how much it should be)
In addition, the examination reveals the presence of blood clots. This symptom indicates the advanced stage of the disease. The thrombus may be located in the superior vena cava. This causes subsequent swelling of the head, neck and upper chest. A clot formed inside the inferior vena cava causes swelling and pain in the legs. Blood clots in the arteries cause hypertension, changes in skin color and subsequent numbness.
Thrombocytopenia: symptoms and treatment
How to determine?
If a laboratory blood test reveals a significant decrease in the number of platelets compared to age norms, the child is diagnosed with thrombocytopenia.
This condition is dangerous for a small organism, since if the epithelium is damaged or internal bleeding occurs, the blood cannot clot, which leads to significant blood loss and a sharp deterioration in well-being (in some cases, even death).
The only way to stop the bleeding may be a transfusion of donor blood with a high platelet count.
To prevent serious consequences, it is important to know the symptoms and signs of thrombocytopenia in children. These include:
- frequent nosebleeds;
- bleeding gums, independent of tooth brushing;
- bruises and small hematomas on the body;
- a small rash that occurs mainly on the legs, ankles, thighs and buttocks (appears in 100% of children with this diagnosis);
- blood streaks in feces and urine.
Separately, it is worth paying attention to cases when even with minor damage to the skin (for example, with a shallow cut), a large amount of blood is observed. This sign almost 100% indicates developing thrombocytopenia.
Causes
A decrease in platelets is not always caused by internal pathologies. There are also external reasons for which signs of thrombocytopenia may be observed in children.
Reasons for decreased platelet count in childhood:
- taking medications (allergy to active substances);
- improper and unbalanced diet with low iron content;
- anemia;
- general intoxication of the body (for example, poisoning with poisons or heavy metals);
- the presence of antiplatelet specific antibodies in blood cells;
- bacterial and viral infections;
- Fanconi syndrome (hereditary form of thrombocytopenia);
- disorders of the thyroid gland;
- insufficient intake of folic acid from food.
Thrombocytosis in children
Thrombocytosis is an increase in the number of platelets in the blood to values several times higher than normal. Most often, thrombocytosis is a consequence of a viral or bacterial infection. In particularly severe cases, an increase in blood cells may indicate the development of cancer.
How to determine: symptoms
The symptoms of thrombocytosis are similar to the clinical manifestations of thrombocytopenia, although there are still some differences. If a child has at least one of the listed signs, you should immediately consult a doctor and take a blood test.
Symptoms of thrombocytosis in childhood:
- frequent and severe nosebleeds;
- blue skin;
- the appearance of subcutaneous hemorrhages;
- itching and burning in certain areas of the skin;
- tingling sensation on the skin;
- cold hands and feet at a comfortable ambient temperature;
- dyspnea;
- increased heart rate.
The child may also complain of frequent headaches. In some cases, pressure surges and blood clots may form.
Causes
To correctly determine the cause of the increase in platelets, it is necessary to diagnose what type of thrombocytosis is developing in the child. The treatment regimen and tactics for managing a small patient will depend on this.
| Type of thrombocytosis | Causes |
| Clonal | Bone marrow stem cell defects |
| Primary | Pathologies in the functioning of bone marrow cells, the formation of several sites of hematopoiesis |
| Secondary |
|
Recommendations for thrombocytosis
- Consult your doctor about the use of products that contain acetylsalicylic acid (for thinning the blood).
- During the day, offer your child compotes and fruit drinks made from blueberries, lingonberries and cranberries as often as possible.
- Monitor the iodine content in the body, and if there is a deficiency, ensure sufficient consumption of fish and seafood.
- If the child does not have problems with the gastrointestinal tract, it is recommended to add fresh garlic and ginger (in minimal quantities) to food.
- In the morning, you can give your baby cocoa without sugar (a prerequisite is that the drink must be consumed on an empty stomach).
- Olive and flaxseed oils, as well as foods rich in magnesium and B vitamins, should be mandatory products in a child’s diet for thrombocytosis.
- Avoid dehydration (the water norm for a child is 1 liter per day).
- Increase the amount of fruits and vegetables (tomato juice and lemons are especially useful).